- Page 1
- Page 2
- Page 3
- Page 4
- Page 5
- Page 6
- Page 7
- Page 8
- Page 9
- Page 10
- Page 11
- Page 12
- Page 13
- Page 14
- Page 15
- Page 16
- Page 17
- Page 18
- Page 19
- Page 20
- Page 21
- Page 22
- Page 23
- Page 24
- Page 25
- Page 26
- Page 27
- Page 28
- Page 29
- Page 30
- Page 31
- Page 32
- Page 33
- Page 34
- Page 35
- Page 36
- Page 37
- Page 38
- Page 39
- Page 40
- Page 41
- Page 42
- Page 43
- Page 44
- Page 45
- Page 46
- Page 47
- Page 48
- Page 49
- Page 50
- Page 51
- Page 52
- Page 53
- Page 54
- Page 55
- Page 56
- Flash version
© UniFlip.com
- Page 2
- Page 3
- Page 4
- Page 5
- Page 6
- Page 7
- Page 8
- Page 9
- Page 10
- Page 11
- Page 12
- Page 13
- Page 14
- Page 15
- Page 16
- Page 17
- Page 18
- Page 19
- Page 20
- Page 21
- Page 22
- Page 23
- Page 24
- Page 25
- Page 26
- Page 27
- Page 28
- Page 29
- Page 30
- Page 31
- Page 32
- Page 33
- Page 34
- Page 35
- Page 36
- Page 37
- Page 38
- Page 39
- Page 40
- Page 41
- Page 42
- Page 43
- Page 44
- Page 45
- Page 46
- Page 47
- Page 48
- Page 49
- Page 50
- Page 51
- Page 52
- Page 53
- Page 54
- Page 55
- Page 56
- Flash version
© UniFlip.com
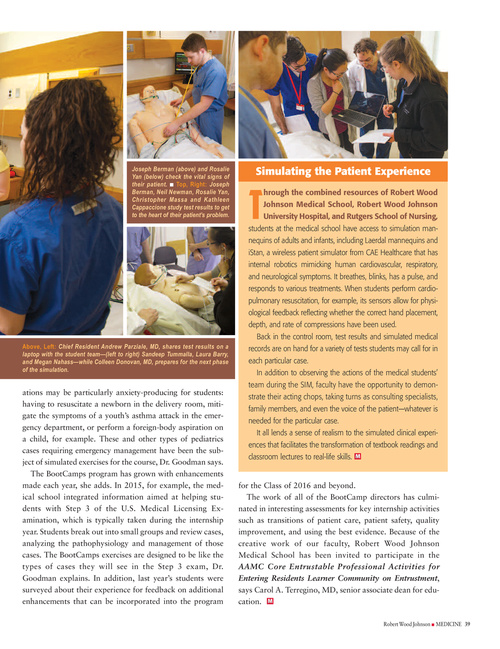
Joseph Berman (above) and Rosalie Yan (below) check the vital signs of their patient. I Top, Right: Joseph Berman, Neil Newman, Rosalie Yan, Christopher Massa and Kathleen Cappaccione study test results to get to the heart of their patient’s problem.
Simulating the Patient Experience
T
hrough the combined resources of Robert Wood Johnson Medical School, Robert Wood Johnson University Hospital, and Rutgers School of Nursing,
students at the medical school have access to simulation mannequins of adults and infants, including Laerdal mannequins and iStan, a wireless patient simulator from CAE Healthcare that has internal robotics mimicking human cardiovascular, respiratory, and neurological symptoms. It breathes, blinks, has a pulse, and responds to various treatments. When students perform cardiopulmonary resuscitation, for example, its sensors allow for physiological feedback reflecting whether the correct hand placement, depth, and rate of compressions have been used.
Above, Left: Chief Resident Andrew Parziale, MD, shares test results on a laptop with the student team—(left to right) Sandeep Tummalla, Laura Barry, and Megan Nahass—while Colleen Donovan, MD, prepares for the next phase of the simulation.
Back in the control room, test results and simulated medical records are on hand for a variety of tests students may call for in each particular case. In addition to observing the actions of the medical students’ team during the SIM, faculty have the opportunity to demonstrate their acting chops, taking turns as consulting specialists, family members, and even the voice of the patient—whatever is needed for the particular case. It all lends a sense of realism to the simulated clinical experiences that facilitates the transformation of textbook readings and classroom lectures to real-life skills.
M
ations may be particularly anxiety-producing for students: having to resuscitate a newborn in the delivery room, mitigate the symptoms of a youth’s asthma attack in the emergency department, or perform a foreign-body aspiration on a child, for example. These and other types of pediatrics cases requiring emergency management have been the subject of simulated exercises for the course, Dr. Goodman says. The BootCamps program has grown with enhancements made each year, she adds. In 2015, for example, the medical school integrated information aimed at helping students with Step 3 of the U.S. Medical Licensing Examination, which is typically taken during the internship year. Students break out into small groups and review cases, analyzing the pathophysiology and management of those cases. The BootCamps exercises are designed to be like the types of cases they will see in the Step 3 exam, Dr. Goodman explains. In addition, last year’s students were surveyed about their experience for feedback on additional enhancements that can be incorporated into the program
for the Class of 2016 and beyond. The work of all of the BootCamp directors has culminated in interesting assessments for key internship activities such as transitions of patient care, patient safety, quality improvement, and using the best evidence. Because of the creative work of our faculty, Robert Wood Johnson Medical School has been invited to participate in the AAMC Core Entrustable Professional Activities for Entering Residents Learner Community on Entrustment, says Carol A. Terregino, MD, senior associate dean for education. M
Robert Wood Johnson I MEDICINE 39