Internal Medicine Residency Program
Review of GME related correspondence
Interviews are conducted virtually for selected applicants between October and January each year. If you are invited to interview with us, you will have the opportunity to learn about our culture and our expectations in the context of a robust clinical learning environment with opportunities for research and career development. During the interview day, you will:
- Meet with members of the residency leadership
- Meet our interns and residents
- Be interviewed by a faculty member
- Have a virtual tour of our facilities
The Internal Medicine Residency Program does not sponsor/offer observerships.
Residency Highlights
Accordion Content
-
Our program will begin reviewing application during the first week of October. We will preferentially review applications from students who sent us gold and silver signals. After
conducting a holistic review of these applications, we will begin to send out invitations in batches as applications are reviewed starting the second week in October. Our interview invitations will be sent through Thalamus on Tuesdays and Fridays after 2pm EDT. Applicants will have 2 business days to respond to interview invitations. Interviews will be conducted from November through January. Signaling will be considered for the interview process alone. We will not use signals in the ranking process.
-
***This section has hidden code and may break if edited.

Payal Davé, MD
Associate Professor of Medicine
Program Director, Internal Medicine Residency
Vice Chair of Clinical Affairs, Department of MedicineThank you for visiting our Program’s website! Our mission is to provide patient-centered education, while promoting professionalism, scholarship and research. We take great pride in the accomplishments of our residents and alumni who embody the core values of our program.
By cultivating an environment that affords opportunities for our residents to be leaders in medicine, we actively engage trainees in all aspects of their professional development. Residents focus on the provision of outstanding patient care, the development and application of a robust knowledge base, and involvement in innovative research. All of this occurs in an environment that remains committed to viewing the practice of medicine as a calling to the service of others.
While time in residency is not sufficient to learn all that internal medicine has to teach, our integrated curriculum sets the framework for education during residency and beyond. This website contains detailed information about our program, and we invite you to peruse this resource.

Jeanne Clark, MD, MPH
Chair, Department of Medicine
Henry Rutgers Professor
Rutgers Health Robert Wood Johnson Medical School -

Payal Davé, MD
Program Director, Internal Medicine Residency Program
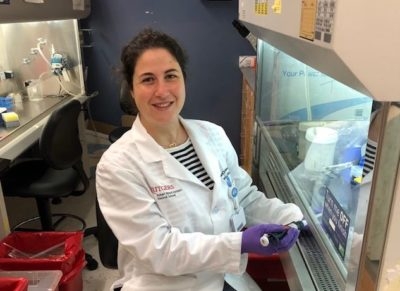
Associate Professor of MedicineDr. Payal Dave is the Program Director of the Internal Medicine Residency Program at Rutgers Robert Wood Johnson Medical School and an Associate Professor of Medicine. A graduate of Rutgers College and the Medical College of Virginia, she completed her residency and chief residency at RWJMS and has been a dedicated faculty member since 2004.
With over two decades of experience in academic medicine, Dr. Dave has shaped the residency program through her leadership in curriculum development, recruitment, and clinical training. She has chaired multiple residency committees, including the Clinical Competency, Resident Recruitment, and Science of Medicine Committees, and has been instrumental in guiding residents through the evolving landscape of medical education.
Dr. Dave is a respected educator and mentor, known for her commitment to humanism and professionalism. She teaches across inpatient and outpatient settings and has led numerous board review sessions, clerkship activities, and residency preparation workshops. Her scholarly work includes publications on cardiovascular health disparities and clinical reasoning, as well as invited talks on residency recruitment at national meetings.
She is actively involved in service at the institutional and community levels, including the Graduate Medical Education Committee, the Eric B. Chandler Health Center, and initiatives focused on South Asian health outcomes. Recognized as a Top Doctor in New Jersey, Dr. Dave continues to advocate for excellence in patient care, education, and equity.

Christina Theodorou, MD
Associate Program Director, Internal Medicine Residency ProgramDr. Christina Theodorou is an Associate Program Director of the Internal Medicine Residency Program at Rutgers Robert Wood Johnson Medical School and an Assistant Professor of Medicine. She graduated from Johns Hopkins University, where she was elected to Phi Beta Kappa, and completed her postbaccalaureate premedical studies at Columbia University. She earned her medical degree from Rutgers Robert Wood Johnson Medical School, where she was elected to the Alpha Omega Alpha Honor Medical Society, and completed her residency in Internal Medicine at Robert Wood Johnson University Hospital.
Since 2020, Dr. Theodorou has served as a core faculty hospitalist on the Medical Teaching Service, supervising residents and medical students. She is a Clinical Coach and History & Physical Advisor for the Internal Medicine Clerkship, a Master Clinician in the M2 Physicianship Course, and she directs the residency’s Cardiology Board Review series. She also leads professional development workshops on clinical reasoning, resident education, and feedback strategies.
Her academic contributions include peer-reviewed research on patient-centered care and manuscript review for medical education journals. She has been engaged in service at multiple levels, with national involvement through the American College of Physicians New Jersey Chapter and institutional roles including Faculty Advisor for Careers in Medicine. Within the residency, Dr. Theodorou chairs the Humanism and Professionalism, Clinical Competency, and Science of Medicine Committees and serves on the Intern Selection and Program Evaluation Committees. She is dedicated to advancing education, mentorship, and the professional development of future physicians.

Christine Fanning, MD, FACP
Associate Program Director and Princeton Site Director, Internal Medicine Residency Program
Academic Hospitalist, Penn Medicine - Princeton Medical CenterDr. Christine Fanning serves as an Associate Program Director and Princeton Site Director for the Rutgers Robert Wood Johnson Medical School Internal Medicine Residency Program and is an Academic Hospitalist at Penn Medicine – Princeton Medical Center. A graduate of New York Medical College, she completed her internal medicine residency and chief residency at Rutgers RWJMS, where she has remained a dedicated educator and clinician.
Since joining the faculty in 2015, Dr. Fanning has held multiple leadership roles, including Site Director for the Internal Medicine Residency at Princeton Medical Center, Core Faculty for the residency program, and Co-Site Director for the Internal Medicine Clerkship. She is also board-certified in both Internal Medicine and Clinical Informatics, serving as a Physician Informaticist and Epic Power User, where she supports clinical decision-making and EHR optimization.
Dr. Fanning is a passionate educator, recognized with multiple Excellence in Teaching Awards and the AΩA Volunteer Clinical Faculty Award. She leads board review sessions, moderates Morbidity & Mortality conferences, and mentors residents and students in both inpatient and outpatient settings. Her scholarly work includes publications on resident wellness, simulation-based education, and healthcare quality improvement.
Active in institutional and professional committees, Dr. Fanning contributes to initiatives in patient safety, sepsis care, resuscitation, and medical education. Her commitment to mentorship, innovation, and compassionate care makes her a vital leader in shaping the next generation of internists.

Bryan Broderick, MD, MEHP
Associate Program Director, Internal Medicine Residency Program
Co-Director of Medical Education Track
Assistant Professor of MedicineDr. Bryan Broderick serves as Associate Program Director for the Internal Medicine Residency Program at Rutgers Robert Wood Johnson Medical School, where he also co-directs the Medical Education Track. A committed educator and clinician, Dr. Broderick brings a strong foundation in academic medicine and a passion for training future physicians.
He earned his medical degree from Rutgers New Jersey Medical School and completed his internal medicine residency at The Johns Hopkins Hospital, where he served as Assistant Chief of Service/Chief Resident. He continued at Johns Hopkins for fellowship training in Pulmonary and Critical Care Medicine and earned a Master of Education in Health Professions with a concentration in educational research, along with a Post-Master’s Certificate in Evidence-Based Teaching.
At Rutgers, Dr. Broderick supervises residents and fellows across inpatient medicine, pulmonary consults, and the ICU. Board-certified in internal medicine, pulmonary disease, and critical care medicine, he is dedicated to delivering compassionate, evidence-based care while fostering clinical excellence through bedside teaching.
His academic interests center on medical education, with active research in diagnostic reasoning, point-of-care ultrasound (POCUS) training, and curriculum innovation. Dr. Broderick has received multiple honors, including the Excellence in Teaching Award from RWJMS and membership in Alpha Omega Alpha.
To learn more about his work and publications, visit BryanBroderickMD.com.

Sarang Kim, MD,
Director of Medical Education Track
Professor of Medicine, Chief of Division of EducationDr. Sarang Kim is the Director of the Medical Education Track for the Internal Medicine Residency Program at Rutgers Robert Wood Johnson Medical School, where she also serves as Professor of Medicine and Chief of the Division of Education. A graduate of the University of Chicago Pritzker School of Medicine, Dr. Kim completed her residency in internal medicine and fellowship in General Internal Medicine at the Hospital of the University of Pennsylvania.
Since joining Rutgers in 2004, Dr. Kim has held numerous leadership roles in medical education, including Clerkship Director, Ambulatory Medicine Director, and Associate Dean for Preclerkship Education. She is a nationally recognized educator and researcher, with peer-reviewed publications and invited presentations on clinical reasoning, assessment, and evidence-based medicine.
Dr. Kim is a Master Educator and recipient of numerous teaching awards, including the Chancellor’s Educator of the Year Award, the Richard A. Harvey Excellence in Innovative Teaching Award, Medical Education Innovator Award, as well as multiple resident teaching awards. She co-founded DR MERL, a widely used medical education literature review platform, and has served on national committees for the AAMC and NBME.
Her clinical work spans inpatient and outpatient general internal medicine, and she is deeply committed to mentoring residents, students, and junior faculty. As Interim Associate Program Director, Dr. Kim brings a wealth of experience in curriculum innovation, faculty development, and learner assessment to support the growth and success of the residency program.
-
***This section has hidden code and may break if edited.

Our Internal Medicine Residency is a community built on belonging which is vital to strengthening our learning and patient care. We foster a culture where every resident feels seen, valued and empowered to bring their authentic self to medicine. An environment of mentorship, collaboration and respect drive excellence in care and learning. Our program is one in which each person belongs, grows and thrives!


-

Inpatient Rotations
Floor teams are structured to include a senior resident (PGY-2 or PGY-3), an intern, a fourth-year medical student (sub-intern) and one or two third-year medical students working closely with their assigned teaching attending in one to two week blocks. Interns care for an average of 8-10 patients at any given time. In addition to weekday didactic conferences and noon report, daily teaching rounds occur at the bedside.
Late call until 8pm, short call until 2pm, and pick up mornings are interspersed to ensure adequate teaching volume, case mix diversity, and preparedness for practice and fellowship training, in a drip model. Experience in the closed Intermediate Care Unit (IMCU) at Princeton, the liquid oncology teaching service at RWJUH, and the Intensive Care Units at RWJUH present opportunities for developing skills that assist with recognizing “sick” patients at a glance, triaging and prioritizing clinical demands, and gaining procedural skills under direct supervision. Dedicated night float teams assume admitting and cross coverage responsibilities for patients on the teaching services at both hospitals. Signout rounds, allow for supervised education during care transitions. Electives and Selectives
Electives and SelectivesOur residency program offers electives in both traditional and nontraditional internal medicine specialties. Electives are available through our faculty practice and various private office settings between New Brunswick and Princeton. Elective time is uninterrupted by any inpatient or clinic obligations and allows our residents to completely immerse themselves in the elective experience. Residents work closely with subspecialty faculty, fellows and fellowship directors, establishing opportunities for mentorship and career counseling.
All interns participate in Geriatric medicine selective while senior residents experience sports medicine, HIV, palliative care, dermatology, weight loss management clinic and the transgender clinic in a combined mandatory selective.
Some of the structured electives offered in our residency program beyond routine subspeciality experiences include : Advanced GI, Congestive Heart Failure, Electrophysiology, Bone Marrow Transplant, Hematologic Pathology, Renal Transplant Medicine, Hypertension and Practice Tailoring (GIM Private Office, Pharmaceutical Industry, Health Care Insurers, etc). For those rare instances when residents seek specialized training not available at our institutions, special arrangements can be made for rotations at external sites on a case-by-case basis.
Electives are available to both interns and residents in one or two week blocks. Electives are free of call and have no weekend coverage obligations. In addition to requesting research blocks, all residents are strongly encouraged to engage in research during their elective rotations and continuity clinic weeks.
 Continuity Office Practices – Ambulatory Curriculum
Continuity Office Practices – Ambulatory CurriculumEach resident is assigned to a general medicine continuity clinic site for the duration of their training.
Residents attend continuity clinic every fifth week for five clinical sessions where they evaluate initial/return visits of patients representing cultural, socioeconomic and disease diversity. Residents are the primary care providers and assume all clinical responsibility for a panel of patients with a broad range of medical conditions under the supervision of dedicated teaching faculty. In addition, residents provide preventive health services, consultation services, preoperative evaluations, and disability determinations for their patients. Population management and quality improvement is built into the clinic experience for all residents.
The mornings during clinic week focus on board review, ambulatory didactics, and EBM education – all moderated by members of the program leadership. Time for subspecialty research and clinical quality improvement is frequently carved out of the schedule. Residents may also avail this time to gain outpatient clinical experience in the future specialty of their choice.
 Rounds
RoundsBedside rounds occur daily at the bedside with dedicated hospital-based teaching faculty at both hospitals.
Conferences:
- Board Review – Daily morning board review facilitated by a member of the program’s leadership conducted during ambulatory clinic week. ACP’s MKSAP modules form the curricular basis for team-based learning.
- Noon Report – Cases presented by interns and residents are moderated by the chief resident and faculty. Innovative presentations and gaming formats are utilized. Medical Jeopardy is a highlight!
- Noon Conference – 45 minute sessions on key topics are delivered by subspecialty faculty.
- Journal Club – Residents deliver weekly journal club presentations where clinically relevant literature is reviewed and research design and methodology is discussed.
- Grand Rounds – Weekly Grand Rounds delivered by nationally renowned experts in the specialty of medicine are conducted throughout the academic year.
- Special Conferences – include a Summer Emergency Lecture series; Morbidity and Mortality; Quality & Safety and Combined IM-Specialty conferences are interspersed throughout the year.
 Competency-Based Curriculum
Competency-Based CurriculumOur curriculum encompasses all the ACGME competencies in the context of the Art, Science and Business of Medicine.
The Art of Medicine curriculum covers a broad range of topics in the areas of implicit bias and microaggressions, physician wellness, medical ethics, communication, cultural and professional competency, and end of life care, to name a few. The format for these conferences include open discussions and case based presentations.
The Science of Medicine curriculum consists of core clinical topics in the areas of General Internal Medicine, Allergy and Immunology, Cardiology, Pulmonary, Nephrology, Gastroenterology, Rheumatology, Hematology, Oncology, Endocrinology and Infectious Disease. These talks are delivered on an annual cycle during noon conference at both our sites by subspecialty faculty. A separate core conference series for the ICU takes place in the ICU.
The Business of Medicine curriculum includes topics related to career options in medicine, healthcare law, coding/billing, care and consultative medicine, personal finances, and employment terms and contracts.
***This section has hidden code and may break if edited. -

The "4+1" Block Schedule
- Our block schedule design completely separates inpatient “service” rotations from outpatient clinic experiences
- Interns and Residents spend 2-4 weeks on service rotations or electives with the 5th week at their continuity clinic site for ambulatory medicine
- More balanced distribution of service rotations throughout the year.
- Allows for a better integrated focus on ambulatory medicine with patient care sessions each afternoon during the +1 week.
- AM sessions during the +1 week are dedicated to the ambulatory curriculum, quality improvement, safety, and EBM.
- About 2/3 of the Inpatient rotations are at RWJUH while 1/3 is at our community affiliate, Princeton Medical Center.
- Vacations are assigned in two week blocks at the PGY 1 level and in one of two week blocks at the PGY 2/3 level.
PGY-1
4 Weeks vacation
10 Weeks of Continuity Clinic
8 Weeks Elective
18 Weeks Inpatient Floors
6 Weeks Night Float
4 Weeks Medical Intensive Care Unit
2 Weeks Intermediate Medical Care UnitPGY-2
4 Weeks vacation
10 Weeks of Continuity Clinic
8 Weeks Elective
12 Weeks Inpatient Floors
4 Weeks Night Float
4 Weeks Medical Intensive Care Unit
4 Weeks Coronary Critical Care Unit
2 Weeks Hematologic Malignancies Inpatient Service
2 Weeks Back-up ResidentPGY-3
4 Weeks vacation
10 Weeks of Continuity Clinic
8 Weeks Elective
14 Weeks Inpatient Floors
4 Weeks Night Float
4 Weeks Medical Intensive Care Unit
3 Weeks Coronary Critical Care Unit
2 Weeks Hematologic Malignancies Inpatient Service
2 Weeks Back-up Resident
1 Week Intermediate Medical Care UnitSchedule at RWJUH
- Drip admission system on floors with 5 floor teams (1 resident, 1 intern)
- 1 Admitting resident
- Long call q5 till 8pm
- Typical non call day is from 7am – 4:30pm
- Backup resident support
- Night Float (Sunday-Friday) 8pm-8:30am
- MICU: Day & night shift teams include residents, fellow & 24/7 intensivist support
- CCU: Day & night shift teams include 2 residents, 1 fellow & 1 attending
- Leukemia & Lymphoma Service: Staffed by 2 residents, 1 Fellow & 1 Attending
Schedule at Princeton
- Drip system on floors with 3 teams (1 resident, 1 intern per team)
- 1 admitting 2 resident team
- Long call q6 till 8pm
- Typical non call day is from 7am-4:30pm
- Night Float (Sunday-Friday) 8pm-8:30am
- Intermediate Care Unit Team: 1 resident & 1 intern team under attending supervision
- No ICU rotations at this site
 ***This section has hidden code and may break if edited.
***This section has hidden code and may break if edited. -
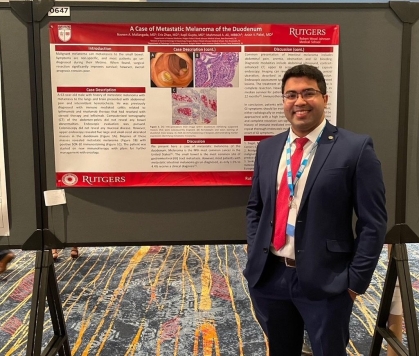
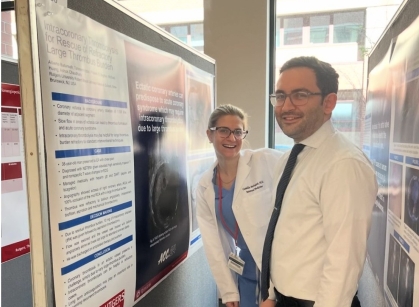
Understanding the important role of robust research during training and beyond, the program established the Residency Research Committee in 1999 to direct and monitor research outcomes of our housestaff. An annual in-house research day and grand rounds is held each year in spring to showcase the work of our residents and fellows and promote research based collaboration.

Certificate in Clinical and Translational Science (CTS)
Categorical residents may choose to obtain a Certificate in Clinical and Translational Science (18 credits) on a part-time basis offered by Rutgers Graduate School of Biomedical Sciences. Courses are conducted once a week in the evening. Coursework for certification includes: Perspectives in Translational Pharmacology, Ethics and Regulations in Clinical Research, Clinical Biostatistics, Epidemiology, Practical Aspects of Clinical Trial Design and Grant Writing for Clinical Research. If selected to enroll in this program, the department of medicine and the school of biomedical sciences will jointly provide full tuition support.

Research with Distinction
The Research with Distinction program launched in 2005 recognizes residents with exceptional research productivity at the time of training completion. The residency research committee has established eligibility criteria.
At graduation, the Certificate with Distinction in Research will be awarded to select residents. This Distinction acknowledges original research undertaken during Internal Medicine training at Rutgers Robert Wood Johnson Medical School. It is not awarded for research done prior to acceptance to residency and cannot be granted for work credited toward any formal degree. This work may be carried out in any field appropriate to Internal Medicine where objective, critical inquiry can be made. Residents are encouraged to publish their research findings in peer reviewed journals.
ABIM Research Pathway
“The ABIM Research Pathway is an integrated program that combines training in research with training in clinical internal medicine and its subspecialties. This pathway is recommended only for physicians who intend to seriously pursue a career in basic science or clinical research. Physicians who are interested in teaching or practicing internal medicine should pursue the standard three years of internal medicine training. Prospective planning for the research pathway by trainees and program directors is necessary. The training experience of all physicians in this pathway will be documented through ABIM’s tracking program. Because this pathway integrates research and training in internal medicine, with or without subspecialty training, entry implies a commitment to its completion. Trainees interested in a research career should work with their residency program director and research mentor to design an appropriate training plan that will provide an adequate clinical experience and meet ABIM’s requirements. Ideally, planning for this pathway should occur during PGY-1, and ABIM should be notified of a trainee’s intention to pursue such training by spring of PGY-2.
The internal medicine program director must be in support of a resident’s request to pursue the research pathway. ABIM requires that candidates for certification in internal medicine are competent in: (1) patient care and procedural skills, (2) medical knowledge, (3) practice-based learning and improvement, (4) interpersonal and communication skills, (5) professionalism and (6) systems-based practice for both the PGY-1 and PGY-2 years of training. Furthermore, the internal medicine program director must coordinate plans for the resident’s training with a research mentor and, if appropriate, the subspecialty program director. It must be clear which program director is responsible for the resident’s training after PGY-2. If the research experience is to be in a subspecialty, the subspecialty program director should become responsible for training through the research pathway beginning in PGY-3. If the research experience is to be in internal medicine, the internal medicine program director should continue to be responsible for training through the research pathway.”
Christoph Buettner, MD PhD
Chief, Division of EndocrinologyPresentations at National Meetings
The program supports (schedule and funding) travel to national meetings as first authors. Our residents have presented their work at the following society meetings over the past 3 years.
- Alliance for Academic Internal Medicine
- American Academy of Endocrinology
- American Association of Clinical Endocrinologists
- American College of Allergy
- American College of Cardiology Conference
- American College of Chest
- American College of Gastroenterology
- American College of Physicians
- American College of Rheumatology
- American Heart Association
- American Medical Association
- American Society of Clinical Oncology
- American Society for Radiation Oncology
- American Thoracic Society
- Asthma and Immunology
- Chest International Annual Conference
- Digestive Disease Week
- Endocrine Society
- Heart Failure Society of America
- ID Week
- Infectious Diseases Society of America
- International Academy of Cardiology
- Society for Cardiovascular Angiography and Interventions
- Society of Critical Care Medicine
- Society of General Internal Medicine
- Society of Hospital Medicine
- Society for Immunotherapy of Cancer
- Society for Melanoma Research



 ***This section has hidden code and may break if edited.
***This section has hidden code and may break if edited. -
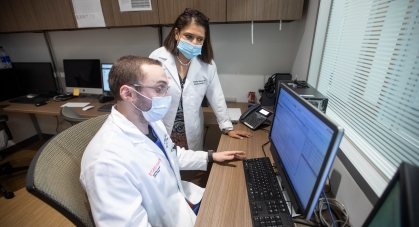
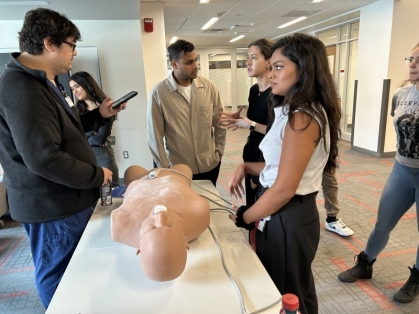
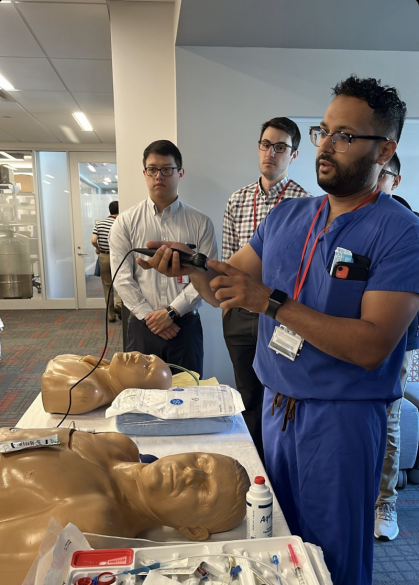
***This section has hidden code and may break if edited.Many aspects of clinical medicine can be taught and evaluated in a simulated setting with the goal of trained execution in live patient care scenarios that include codes, complex care triages, and executing decisions in systems derived interdisciplinary teams. The performance feedback loop is a critical part to any successful intervention. During clinic week and noon conference, residents engage in simulation exercises in replicas of patient rooms that include high fidelity mannequins with monitors that present objective patient data. Control desks with trained personnel, real time observation windows and multidisciplinary debriefing are a part of the exercise. Residents practice managing acutely unstable patients and engage in diagnostic reasoning exercises in small groups of 3-4 residents with peers, faculty leaders from Pulm-CCM medicine, and IM core faculty/chief residents. A strong emphasis is placed on teamwork and collaboration between residents, nursing, respiratory therapists and pharmacists with physical supervision.

-
***This section has hidden code and may break if edited.

Clinical Research Track
Goal
The Clinician Research Track (CRT) was established to provide selected and highly motivated residents in the residency program with opportunities for research that include skill-building didactic and group sessions with mentored research experiences. Over the past five years, our residents have used the CRT’s hands-on, mentored education as a steppingstone to advance their clinical and research careers.
Curriculum
The curriculum consists of:
-
Didactic and group sessions (2 hour sessions every 5 weeks)
-
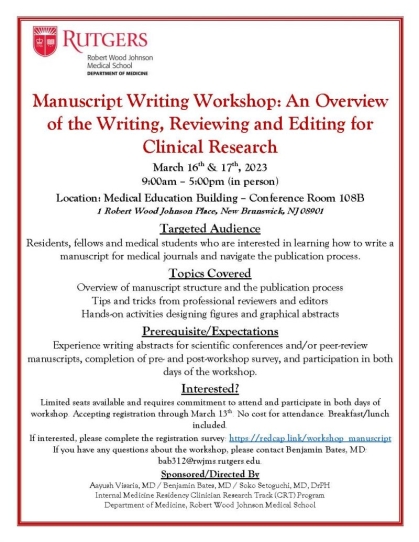
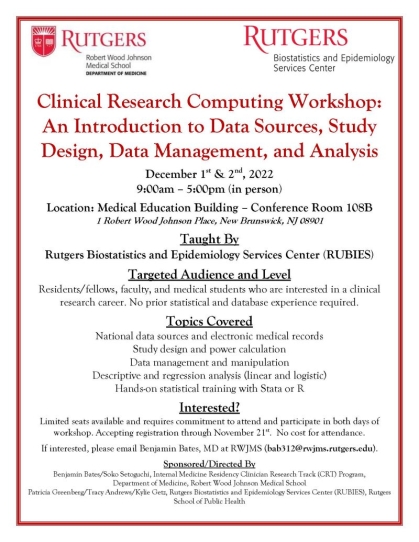
Rigorous, clinically-focused workshops (2 days per workshop, each once per year). Ongoing workshops include clinical data analysis, systematic review/meta-analysis, and manuscript writing.
-
Mentored research with protected research elective weeks (minimum of 4 weeks and maximum of 8 weeks per year).
Didactic Sessions
Selected topics in clinical research will be provided as didactic sessions (in person session and video recording) every 5 weeks throughout the year (July-June)
Topic
Instructor
Introduction and Overview of Clinical Research study designs
Brian Strom
Bias and Confounding
Tobias Gerhard
Introductory biostats from a clinical researchers perspective
Daniel Horton
Clinical research leveraging big data
Soko Setoguchi
Means and methods of primary data collection
Intro to ‘omics’
Fred Wondisford
Clinical trials
Jeffrey Carson
Cost and cost effectiveness analyses
Laura Pizzi
Introduction to mixed methods research
Benjamin Crabtree
Introduction to translational research
Reynold Panettieri
Group Sessions/Hands-on Sessions
All clinician researcher track residents will meet for 2 hours every 5 weeks for a group discussion session. The group session will provide a hands-on learning experience in research related topics including literature search, IRB navigation, data sources, data management and analysis, abstract writing, effective scientific presentation, and manuscript writing while providing opportunities for presentations and discussion of individual research projects among peers, researchers and research mentors.
Workshops
Each trainee in the Clinician Research Track will participate in workshops designed to advance their knowledge and skills in clinical research. Currently, we offer three workshops each year: (1) clinical data analysis workshop; (2) systematic review and meta-analysis workshop; (3) manuscript writing workshop. Each workshop provides a detailed review of the subject and are designed to be educational for trainees of all levels. Below are example flyers from the most recent workshops. New workshops are in development and requests are always appreciated!
Mentored Research
Each resident in this firm will be guided and matched to a research mentor based on his or her research interests. The clinician researcher track resident will be guided by his/her mentor to identify projects that will be supported by their mentor’s research program and will conduct hands-on research projects that are likely to yield high quality research for publication as abstracts/manuscripts. The residents will utilize 4-8 elective weeks each year as research electives to conduct mentored projects. In addition, each resident will be matched to a Masters student in Biostatistics at the Rutgers School of Public Health (RSPH). This student will collaboratively work with the resident under the guidance of their statistics mentor at RSPH to support data analyses for residents’ projects.
Pre-requisites
-
Clinical research experience
-
Plan to lead and collaborate in clinical research during and following residency
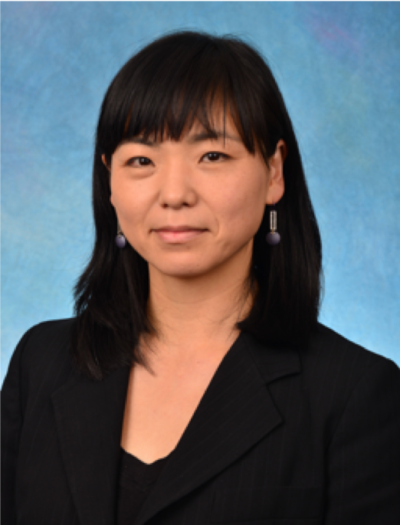

RESEARCH TRACK DIRECTOR
Soko Setoguchi, MD, DrPH, a cardiologist by training, board-certified general internist, and epidemiologist, is Associate Professor of Medicine and Epidemiology, Rutgers Robert Wood Johnson Medical School (RWJMS) and at Rutgers School of Public Health. She serves as the Director of Clinical Research Education in Department of Medicine. She is also the new Co-Director of the Master of Science in Clinical and Translational Science (MS-CTS) at Rutgers School of Graduate Studies. After her medical school and training in Cardiology in Japan, she completed her doctoral training in epidemiology at the Harvard School of Public Health. She was on the research faculty in the Division of Pharmacoepidemiology at Brigham and Women’s Hospital/Harvard Medical School and at Duke Clinical Research Institute before she completed US residency training in Internal Medicine at University of North Carolina Hospital and then RWJMS. Dr. Setoguchi is an international leader in the field of pharmacoepidemiology, the study of the health effects of medications and other medical products in populations. She has authored more than 120 peer-reviewed papers in leading medical journals and has been funded by both federal and non-federal sources for her pharmacoepidemiology research program. Her research uses large databases to perform health services and outcomes research and comparative effectiveness research for medications and implantable medical devices in patients with chronic disease.
RESEARCH TRACK, ASSISTANT DIRECTOR
Benjamin Bates is a general internist and board certified in Internal Medicine. After Internal Medicine Residency, he completed a two-year research fellowship in cancer pharmacoepidemiology and health services research. His research focuses on the treatment and health outcomes of patients with cancer. He has received support from the New Jersey Commission on Cancer Research, the Robert E. Leet and Clara Guthrie Patterson Trust Mentored Research Award, and the National Cancer Institute to advance his career as a physician scientist focused on the overall care and health outcomes of patients with cancer. Most recently, he received the Cancer Institute of New Jersey Cancer Survivorship Research Centers Pilot Award Program Cancer Center Support Grant (P30CA072720) to support research on primary care involvement during and following cancer treatment. His manuscripts have been accepted into Journal of Clinical Oncology, Annals of Internal Medicine, and Circulation: Cardiovascular Quality and Outcomes, and he has presented his research at national and international conferences. He was selected as an Editorial Fellow for the ASCO Journals Editorial Fellowship (2022-2023).
More information about his experience as an editorial fellow can be read here: Bates’ ASCO Journals Editorial Fellowship Experience. -
-
The Medical Education Track was launched in 2023 to train our residents who are passionate about teaching to be well prepared for a career in academic medicine. Through small group discussions, workshops, and hands-on teaching experiences across diverse learning environments, residents in the Med Ed Track gain the knowledge and skills necessary to help them succeed as leaders in medical education.
Med Ed Track Program Objectives
At the conclusion of the Medical Education Track, residents will:
-
Gain a basic understanding of major theoretical frameworks in medical education.
- Learn and apply common teaching, feedback, and coaching techniques across diverse learning environments.
- Accumulate over 100 hours of hands on teaching experience.
- Recognize and pursue opportunities for educational innovation, with the option to present at regional or national educational conferences.
Program requirements
- Satisfactory performance in all ACGME competency domains and Milestones evaluations.
-
Commitment to participating in Med Ed Track activities while on ambulatory week (beyond the AM curriculum didactic time).
- Participate in Med Ed Track elective rotations (1 or 3 weeks per year depending on PGY level)
Curriculum
- Didactic sessions on core topics in medical education including those related to learning theory, assessment, feedback, coaching, and curriculum development, among others.
- Workshops to practice a variety of teaching and feedback techniques.
- Classroom and bedside teaching involving varying levels of learners and group sizes to teach physical diagnosis, clinical reasoning, or clinical topics.
- Direct observation and feedback by faculty and peers.
- Career exploration and mentoring from established leaders in medical education, including meetings with invited guests from outside institutions.


-
-
***This section has hidden code and may break if edited.
Our Mission
To inspire and prepare the next generation of physician leaders and executives by bridging the gap between clinical medicine and management, pharmaceuticals, innovations, consulting, informatics, payors and venture capital.
Core Curriculum
The curriculum consists of:
- Didactics & Discussion sessions
- Professional Speakers
- Experiental Learning & Internships
- Hackathons & Competitions
The residents must commit to the program for a minimum period of 1 year and are strongly encouraged to enroll for the three-year training period.
Didactics & Discussion Sessions
Business of Medicine Course @ www.headmirror.com, by Ashley Nassiri MD, MBA, Matthew L. Carlson, MD and David S. Haynes, MD, MMHC.
We use the business of medicine curriculum developed by Ashley Nassiri, MD, MBA in podcast format where she has discussions with national/international experts in the areas of leadership, care delivery and practice management.
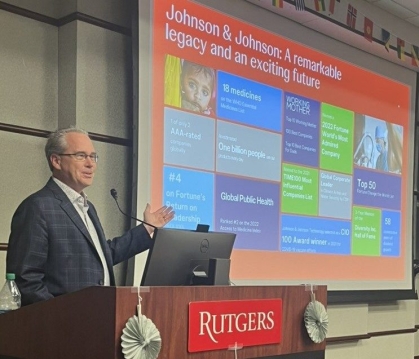
The podcast format gives residents flexibility to listen and learn at their convenience and individual pace. The podcasts are assigned every few weeks and followed up with discussions during dedicated time on ambulatory blocks. Completion of the course results in 19 credits of CME.Professional Speakers
During each ambulatory block, leaders, including program alumni, from a variety of healthcare fields involving clinical medicine, pharmaceutical industry, healthcare consulting and start-ups, informatics and AI, venture capital, and payors are invited to give interactive presentations to our residents. These platforms are invaluable for real world learning, networking, and mentorship.
Experiential Learning and Internships
Practice tailoring experiences are an integral part of the curriculum. Our program provides opportunities to use elective time to explore learning venues beyond traditional clinical medicine. Examples of current partnerships include electives at Horizon Blue Cross/Blue Shield of NJ, Hospital C-Suite shadowing, Bio-Pharma rotations, etc.
Hackathons and Competitions
We support residents in exploring interests in healthcare innovation through hackathons and competitions. In 2022, our RWJMS team won 1st place and grand prize at the Yale CBIT Healthcare Hackathon – BaroCor, an innovative medical device aimed at reducing congestive heart failure exacerbations. These events spark creativity, promote team building skills and offer a wide array of networking opportunities.
Curriculum
Topics covered during the academic year include:
-
Drivers of healthcare expenditures
-
Physician roles in the Pharmaceutical Industry
-
Pharmaceutical costs and affordable medicine
-
Healthcare Consulting
-
Healthcare and Biotech Start Ups & Investments
-
Medical Informatics, IT and Health System Efficiencies
-
Hospital Administration / Path to Chief Medical Office
Healthcare Leadership Track Director

Jay Naik, MD
Jay Naik, MD, is Assistant Professor of Medicine and Vice Chair for Clinical Innovation at Rutgers Robert Wood Johnson Medical School. As Director of the Healthcare Leadership and Management Track, he helps residents develop skills in leadership, innovation, and the business of medicine.
Through a hands-on curriculum, residents explore how clinical practice connects with technology, AI, entrepreneurship, and health systems. Dr. Naik also co-founded the Rutgers Health Hack, where residents collaborate with industry-leading partners like Microsoft, Oracle, Amazon, and Nokia Bell Labs to bring technology innovations into healthcare. Passionate about teaching and mentorship, Dr. Naik has received multiple Excellence in Teaching Awards and is committed to preparing residents to become not only outstanding clinicians but also leaders who shape the future of medicine.
For more information on the Rutgers Health Hack, visit RUhealthhack.com. -
Our stellar residents consistently match into competitive fellowships every year. Take a look at their destinations from 2017 - 2024.
-
***This section has hidden code and may break if edited.
“Our well-being and the well-being of our teams ultimately affects the health and well-being of our patients and our communities.” M. Rapley, MD, AAMC
Individual response to stress and challenge can be variable and unpredictable. A growing body of literature has shed light on increasing rates of burnout among medical students, residents and practicing physicians across disciplines. Developing strategies to build resilience using internal and external resources to nurture and restore “joy” to the practice of medicine remains a critical objective.
Our Wellness Program serves to build peer to peer and vertically integrated support systems. ACTIVE DOCS, teambuilding events, off site retreats, social gatherings and invited speakers and panels serve to educate, integrate and empower our trainees to promote wellness. Mental health and counseling resources are readily available to our trainees and their families.









-
***This section has hidden code and may break if edited.
Accordion Content
-
Recognizing the importance of cultural, socioeconomic and case-mix diversity, residents in training have the opportunity to learn and care for a wide variety of populations that characterize Central New Jersey. A 965-bed tertiary level university hospital and a 300-bed true community hospital, along with exposure to an NCI designated Comprehensive Cancer Center (Rutgers Cancer Institute), and a wide-array of integrated research opportunities at Rutgers, creates a robust training ground for our residents.
Robert Wood Johnson University Hospital (RWJUH) and the Penn Medicine Princeton Medical Center (PMPMC) form the core teaching hospitals for our residency training program in Internal Medicine.

Robert Wood Johnson University Hospital (academic medical center for the RWJ Barnabas Health System)
RWJUH is a 965-bed hospital which provides primary, secondary and tertiary levels of care to central New Jersey and the surrounding areas. The hospital is staffed by full-time faculty in every department, along with a large group of private faculty. The Internal Medicine Department at RWJUH has approximately 140 full-time faculty and 500 community based physicians with clinical teaching interests. An active transfer service brings severely ill and complex patients to RWJUH, allowing for superb training of residents with a large volume of tertiary patients.
For more information: Robert Wood Johnson University Hospital
About New Brunswick: New Brunswick, NJ

Rutgers Robert Wood Johnson Medical School
As one of the nation’s leading comprehensive medical schools, Robert Wood Johnson Medical School is dedicated to the pursuit of excellence in education, research, health care delivery, and the promotion of community health. In collaboration with Robert Wood Johnson University Hospital, the medical school’s principal affiliate, they are recognized as New Jersey’s premier academic medical center. In addition, Robert Wood Johnson Medical School has 34 other hospital affiliates and ambulatory care sites throughout the region. Robert Wood Johnson Medical School encompasses 20 basic science and clinical departments, and hosts centers and institutes including The Cardiovascular Institute, the Crohn’s and Colitis Center of NJ, the Child Health Institute of New Jersey, the Center for Advanced Biotechnology and Medicine, the Environmental and Occupational Health Sciences Institute, and the Stem Cell Institute of New Jersey. The medical school maintains educational programs at the undergraduate, graduate and postgraduate levels for more than 1,500 students on its campuses in New Brunswick and Piscataway and provides continuing education courses for health care professionals and community education programs.

Penn Medicine at Princeton Medical Center (PMPMC)
PMPMC is an excellent 300-bed community hospital, with full-time faculty and private physicians in the Department of Medicine. PMPMC has the advantages of a true community hospital, allowing our medical residents to train in the mainstream primary care setting. The teaching faculty are drawn here by the ideal setting, the presence of the high quality residents and the superb patient pathology that has consistently characterized PMPMC.
For more information: Penn Medicine Princeton Medical Center
About Princeton: Princeton, NJ
Rutgers Cancer Institute of New Jersey (CINJ)
The Rutgers Cancer Institute, established in 1990, is New Jersey’s only National Cancer Institute – designated Comprehensive Cancer Center. Rutgers Cancer Institute delivers advanced comprehensive care to adults and children and conducts cutting edge cancer research. Our housestaff work closely with oncology fellows and faculty during their rotation on the hematologic malignancy service and participate in electives at the outpatient specialty clinics at Morris Cancer Center. Many residents collaborate with faculty on clinical and basic science research projects.
For more information: http://www.cinj.org
***This section has hidden code and may break if edited. -
Each resident is assigned to a general medicine continuity clinic site for the duration of their training. Residents attend continuity clinic every fifth week (+1 week) where they evaluate initial/return visits of patients representing cultural, socioeconomic and disease diversity. Residents are the primary care providers and assume all clinical responsibility for a panel of patients with a broad range of medical conditions under the supervision of dedicated teaching faculty. In addition, residents provide preventive health services, consultation services, preoperative evaluations, and disability determinations for their patients.

Eric B. Chandler Health Center
EBCHC is a comprehensive, Federally Qualified Health Center, jointly operated by the Robert Wood Johnson Medical School and Eric B. Chandler Community Board, Inc.
- Opened in October 1987
- Dedicated to the memory of Dr. Eric B. Chandler, an active and respected community leader recognized for his work in the NAACP and a member of the Board of Directors of the Urban League of Greater New Brunswick
- Primary care services available at Chandler include: family medicine; internal medicine; infectious disease (HIV counseling, testing, and treatment); pediatrics (including EPSDT and child well-care); obstetrics and gynecology; podiatry; family planning; and dentistry (including preventive, restoration, and curative).
- Other services of the center include social services, community outreach, nutrition, and health education.
- On-Site Laboratory services are offered as well.

Zufall Health Center
The Zufall Health Center at Plainsboro is also a Federally Qualified Health Center that provides comprehensive community healthcare services to uninsured and underinsured residents, including mental health services for patients whose physical illnesses are complicated by mental health problems.
- Opened in 2012 with 21 exam rooms, transitioned to Zufall ownership in 2021 with expanded sevices
- Care provided by board certified physicians, highly trained residents, certified nurse midwives, nutritionists, social workers and health educators
- Houses Adult Medical, OB/GYN, Pediatric Clinics as well as providing Podiatry and Dental Services
- More than 22,000 patient visits each year
For more information, click here.
 Rutgers Health at Robert Wood Johnson Medical School
Rutgers Health at Robert Wood Johnson Medical SchoolThis is one of the largest multispecialty physician practices in the state, with more than 500 physicians with expertise in 200-plus subspecialty clinical programs, we provide a full range of highly specialized services for children and adults. It is located in the Clinical Academic Building adjacent to the hospital.
Members of the division of general internal medicine whose focus is on outpatient primary care, practice in this setting. 15 internal medicine residents are assigned to this clinic and conduct their group practice under the direct supervision of GIM faculty. Access to faculty specialists across disciplines is readily available.
***This section has hidden code and may break if edited. -

The Internal Medicine Residency Program offers a uniform package of benefits consistent with those provided at all graduate medical educational programs operated by the medical school. Full details regarding benefits and salary are continuously updated by the Office of Graduate Medical Education.
Benefits
- Book Allowance – $1,300.00 annually
- Professional liability coverage for all activities that are approved components of the residency program
- Life insurance coverage equal to 3 times annual salary
- Housestaff and immediate family members are provided with health insurance effective the first day of the month following two months of employment (60 days). Health care contributions are a percentage of premium based on the housestaff salary, plan and level of coverage.
- Dental Insurance is available – contributions are based on housestaff salary, plan and level of coverage.
- Prescription drug plan is available
- White coats and laundry services
- Vacation: 4 weeks per contract year
- Sick time: 12 days per contract year
- Eight holidays
- Four Personal days (or FH)
- Union – Committee of Interns and Residents Union (CIR) membership optional
- Parking is available at all training sites
- The Employee Assistance Program is a free, confidential resource available through University’s Behavioral Health Care program.
-
Program Coordinators
Peggy Morgan – morganma@rwjms.rutgers.edu
Rachel Stewart – r.stewart@rutgers.eduMailing Address
Internal Medicine Residency Program
Department of Medicine
125 Paterson Street
New Brunswick, NJ 08901(732) 235-8887