The SIDS Center of New Jersey
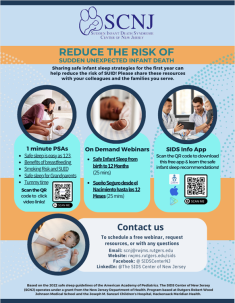
SIDS Center of NJ Free Sleep App
Download the SIDS Center of New Jersey’s English/Spanish award-winning and free mobile phone app that helps families learn and share information about reducing the risk of Sudden Infant Death Syndrome (SIDS) and other sleep-related infant deaths.
Defining Sudden Infant Death Syndrome (SIDS)
What is Sudden Infant Death Syndrome (SIDS)?
- Sudden Infant Death Syndrome (SIDS) is a sudden death in the first 12 months of life that remains unexplained even after a thorough evaluation. It is one of the leading causes of infant mortality.
- Research continues into possible causes of SIDS. However, although causes may not yet be detectable, a great deal is now known about how to reduce the risk of these deaths. This information is described in the 2022 American Academy of Pediatrics Recommendations for Reducing Infant Deaths in the Sleep Environment.
- These evidence-based recommendations also reduce the risk of two other sleep-related infant deaths: accidental suffocation and strangulation in bed and ill-defined and unknown causes.
- Grouped together, these sleep-related infant deaths are called Sudden Unexpected Infant Death (SUID).
- Reduced rates of Sudden Unexpected Infant Death (SUID) can be achieved through using safe infant sleep practices, avoidance of smoke and nicotine exposure during pregnancy and after birth, in addition to other recommendations. Adverse social and health determinants such as preterm birth and delayed onset or absence of prenatal care also affect risk.
Our Mission

Established in 1988, the Mission of SCNJ is to:
- Study the causes and risk factors associated with Sudden Unexpected Infant Death.
- Develop and offer risk reduction education and resources.
- Provide bereavement support to grieving families.
Did you know?
- New Jersey’s rate of SUID is among the lowest in the US
- Established in 1987, the SCNJ collaborates with national and state health, social service, home visiting, and community programs and providers and many other groups to advance the shared public health mission of improving the well-being of NJ’s infants!
- Research by the SIDS Center of New Jersey contributed to the risk reduction guidelines of the American Academy of Pediatrics!
Contact Us
Office: 732-249-2160
Email: scnj@rwjms.rutgers.edu
In-State Hotline: 800-545-7437
The SCNJ operates under a grant from the New Jersey Department of Health and is based at Robert Wood Johnson Medical School and the HMH Joseph M. Sanzari Children's Hospital.
SIDS Center of NJ Free Sleep App
Download the SIDS Center of New Jersey's award-winning and free mobile phone app that helps families learn and share information about safe infant sleep and other risk-reducing recommendations.
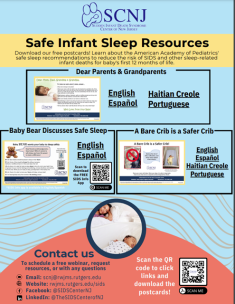
SIDS Center of NJ Education Resources
SCNJ Safe Sleep Videos
ENGLISH
Safe sleep easy as 1, 2, 3
Smoking increases the risk of SUID:
Safe sleep tips for grandparents
Benefits of Breastfeeding
Tummy Time
A brief review of Safe Infant Sleep Guidelines
SPANISH
Riesgo de fumar y SUID
Sueño seguro para los abuelos
Dormir seguro es tan fácil como 1, 2, 3
Beneficios de la lactancia materna para reducir el riesgo de SUID
Tiempo boca abajo
NICHD Safe to Sleep Campaign Resources
NICHD Safe Sleep for Your Baby - English
NICHD Safe to Sleep booklets also can be downloaded in other languages
NICHD Videos:
Safely Keeping Baby Warm: A Q & A on Bedding, Clothing, and Sleep-Related Infant Death
Human Milk, Breastfeeding, and Safe Infant Sleep
Resources for helping families live tobacco-free:
Mom’s Quit Connection
Helpful Safe Sleep Websites:
National Institute of Child Health and Human Development
Safe to Sleep Campaign
Cribs for Kids
SIDS Center of New Jersey Facebook Page
Additional Resources for Providers
American Academy of Pediatrics Updated 2022 Recommendations for Reducing Infant Deaths in the Sleep Environment
On Demand CEU Webinar for Nurses
Safe Infant Sleep Checklist for Providers
Questions and Answers about Safe Infant Sleep for the First 12 Months of Life
This information is based on the Updated Safe Sleep Guidelines of the American Academy of Pediatrics published in Pediatrics in July, 2022.
Discuss these guidelines with your infant's health care provider.
Accordion Content
-
The American Academy of Pediatrics (AAP) informs us that in the United States about 3,500 infants die each year in the first 12 months of life from what are called sleep-related infant deaths. Among these deaths is a grouping termed Sudden Infant Death Syndrome or SIDS. SIDS is the leading cause of infant mortality between 1 and 4 months of age. It is a diagnosis given when a sudden death cannot be explained even after a thorough case investigation that includes a scene investigation, autopsy, and review of the clinical history. But even though the causes may not yet be identified, we have learned what can be done to reduce the risk of these deaths. These evidence-based recommendations are grouped together in the AAP publication, Sleep-Related Infant Deaths: Updated 2022 Recommendations for Reducing Infant Deaths in the Sleep Environment.
These same recommendations also reduce the risk of two other types of sleep-related infant deaths: Ill-defined and Unknown Causes and Accidental Suffocation and Strangulation in Bed. Grouped together, SIDS, Ill-defined and Unknown Causes and Accidental Suffocation and Strangulation in Bed form a category of infant mortality called Sudden Unexpected Infant Death (SUID). By following the recommendations, everyone who takes care of a baby has the power to reduce the risk of these deaths. Share them with everyone who takes care of your baby! The responses to the questions below are based on the AAP safe sleep guidelines.
-
Most SIDS deaths occur in babies between 1 and 4 months of age. More than 90% of all SIDS deaths occur by 6 months of age. However, although it is less common after 8 months of age, parents and caregivers should continue to follow safe sleep practices to reduce the risk of SIDS and other sleep-related infant deaths until a baby’s first birthday.
-
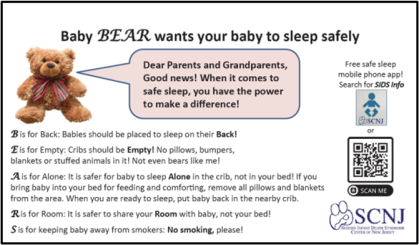
First, babies should be put to sleep on their backs. The use of the back to sleep position has resulted in a major decline in sleep-related infant deaths. Neither the side position nor the belly down position is recommended for placing an infant to sleep. Grandparents may remember that they were advised to do the opposite, to put the baby to sleep on the tummy. However, we know better now, so we do better. Back is best. Check with baby's pediatrician or other health care provider for additional confirmation.
-
There has been no increase in choking or similar problems for babies who sleep on their backs. The AAP states that, "The supine sleep position on a flat, non-inclined surface does not increase the risk of choking and aspiration in infants and is recommended for every sleep, even for infants with...reflux.” For any questions, check with baby's health care provider.
-
The AAP recommends that you place your baby on his or her back at the start of all sleep periods in the first year of life. As they develop, a baby may turn over to another position during sleep. Once babies reach the age where they can roll from back to belly and from belly to back on their own, usually by around six months, they can remain in the position they assumed.
-
To help protect a baby from the risk of a flat spot, the AAP recommends offering lots of tummy time for babies when they are awake and being watched by their parent or caregiver. Tummy time can begin once baby comes home from the hospital of birth. An early goal is to increase the time so that baby receives at least 15 to 30 minutes of supervised tummy time by 7 weeks of age. Also, it is important to make sure that baby isn't spending all his or her time in a crib, or a car seat or an infant carrier. Pick baby up, spend time holding baby and enjoying cuddle time.
-
-
1. The AAP recommends placing infants to sleep in a crib, portable crib, bassinet or play yard that meets current safety standards of the Consumer Product Safety Commission. (https://cpsc.gov/SafeSleep)
2. It should contain a flat, firm mattress. An inclined mattress is considered unsafe. There have been recent recalls of inclined sleepers. A firm mattress means one that returns quickly to its original shape if pressed on.
3. The mattress should be the type intended for the crib or other recommended sleep product being used.
4. There should be no gaps between the mattress and the sides of the crib or other recommended sleep product.
5. The mattress should be covered just by a tightly fitted sheet. The corners of a firm mattress should not curl up when a properly sized sheet is fitted onto on a firm mattress.
6. Don't place any pillows or quilts over or under the sheet.
7. In fact, and this is very important, there should be no loose bedding in the crib. No pillows, no quilts, no blankets, no stuffed animals or other soft or fluffy items, and no bumpers either. Although these things are pretty, they are associated with an increased risk of sleep-related infant deaths. And there should be no one else in the baby's crib or similar safe sleep space.
8. The AAP recommends that babies are safest sleeping near the parent's bed but not in the parent's bed. When the baby is close by the parent's bed, the parent can still see, touch, hear and respond to the baby. Room sharing instead of bed-sharing is best and can reduce the risk of SIDS by as much as 50%. Parents are urged to share their room with their infant for at least the first six months.
9. Parents may choose to bring the baby into bed to play, comfort, cuddle and feed! But, when parents are ready to fall asleep, it is safest to place the baby back in his or her own near-by crib or similar safe sleep space. The longer a sleeping adult shares a bed with baby, the higher baby’s risk for suffocation and other sleep-related deaths.
10. Sometimes a tired parent who is breastfeeding at night may fall asleep with the baby in the adult bed. To keep baby as safe as possible until the parent wakes up and puts the baby back into his or her own nearby sleep space, parents should make sure that their own soft bedding, such as pillows or blankets and even pets are out of reach of the baby so that there is no risk that they will cover the baby's face and cause harm. The baby should be put back into his or her nearby safe sleep space as soon as the parent wakes up. The longer an adult shares the bed with a baby, the higher the baby’s risk for suffocation and a sleep-related deaths.
11. Sleeping in an adult bed with baby (bed sharing) is especially dangerous if the parent: a) has impaired alertness or reduced ability to arouse because of being very fatigued or using sedating medications or substances such as alcohol or illicit drugs; b) smokes cigarettes or uses tobacco products, even if they do not smoke in bed; c) if a very soft surface is used, such as a waterbed, old mattress, a mattress with memory foam, a sofa, a couch, or an armchair. Other situations that add to the risk of bed sharing are a baby less than four months of age, sleeping with someone who is not the infant's parent, a premature or low birth weight baby, or a bed with soft bedding accessories such as pillows or blankets.
12. Sofas and chairs are not designed for babies to sleep on whether alone or with someone and are very dangerous. Babies should not be put to sleep on these. Also, sitting devices such as car seats, strollers, swings, and infant carriers and infant slings are not recommended as baby’s regular sleep space, particularly when the infant is less than four months of age. When an infant falls asleep in a sitting device, move them to a crib or other appropriate flat surface as soon as it is safe and practical to do so. Do not leave infants unattended in car seats and similar items. Also, when using a car seat, avoid letting baby sit slumped over with their chin on their chest.
-
-
Infants should be dressed appropriately for the environment, with no more than one layer more than an adult would wear to be comfortable in that environment. If parents feel that more warmth is necessary, an extra layer of clothing or a type of sleep clothing called a wearable blanket should be used instead of a blanket. It should be the right size for the baby. Parents should avoid overheating the baby because overheating is a risk factor for SIDS. You can tell if a baby is overheated by checking if they are sweating or if the chest feels hot to the touch. Over-bundling and covering the face and head should be avoided. When indoors, infants should not be wearing a hat. Wearable blankets should not contain weighted material, The AAP advises against any baby clothing that contains weighted material.
-
Smoking contains nicotine which has been found to be a major risk factor. Therefore, smoking and exposure to nicotine from any source should be avoided in pregnancy and after. Smoking by a pregnant mother or by people in her presence can cause harm to the developing baby. Exposing the baby to smoke after he or she is born also is a major risk factor. If a mother has stopped smoking during pregnancy to protect her baby, she should stay smoke-free even after! Household smoke matters too. Homes and even cars that contain a baby should be smoke-free zones. In addition to avoiding nicotine, the AAP advises that alcohol, marijuana and opioids also should be avoided during pregnancy and after birth.
-
Yes! Breastfeeding or pumped human milk is associated with a lower risk of SIDS! Therefore, for that reason and many others, providing human milk is highly encouraged. The longer a baby receives breast milk, the lower the risk of SIDS.
-
Pacifiers help reduce risk. If the baby is breastfeeding, parents should wait until breastfeeding is well established before introducing the pacifier. The pacifier should not be attached to baby’s clothing, blanket, stuffed animal, or other item due to the risk of strangulation or suffocation. It should be clean, with nothing coating it, and in good condition. It should be offered but not forced. If it falls out during sleep, you don’t need to put it back in.
-
Even though swaddling does not reduce the risk of SIDS, some parents use it because they feel their babies are calmer and sleep better. If a parent chooses to swaddle, continue to follow safe sleep guidelines. Be sure that baby is placed on his or her back on a firm flat surface. Stop swaddling as soon as babies gives a sign that they are attempting to roll over, usually around three months of age, but it may occur earlier. Do not use weighted material and avoid overheating baby.
-
According to the AAP, “Direct-to-consumer heart rate and pulse oximetry monitoring devices, including wearable monitors, are sold as consumer wellness devices. A consumer wellness device is defined by the Food and Drug Administration (FDA) as one intended “for maintaining or encouraging a healthy lifestyle and is unrelated to the diagnosis, cure, mitigation, prevention, or treatment of a disease or condition.”1 These devices are not required to meet the same standards as a medical device. If a parent chooses to use a monitor at home, it should not be considered a substitute for following AAP safe sleep guidelines. Regarding any device, the AAP, the FDA and the CPSC concur that manufacturers should not claim that a product or device protects against sleep-related infant death unless there is scientific evidence.
-
1. U.S. Department of Health and Human Services, Food and Drug Administration, Center for Devices and Radiological Health. General Wellness: Policy for Low Risk Devices. Guidance for Industry and Food and Drug Administration Staff. Washington, DC: U.S. Food and Drug Administration; 2019
-
-
Get regular medical care throughout pregnancy. Follow baby’s healthcare provider’s advice on vaccines, checkups, and other health issues.
Discuss these AAP guidelines with the infant's health care provider.
Who We Are
Thomas Hegyi, MD
Medical Director, SIDS Center of New Jersey; Director, Neonatal-Perinatal Medicine Fellowship Program; Vice Chair and Professor of Pediatrics, Robert Wood Johnson Medical School, New Brunswick, NJ
Barbara M. Ostfeld, PhD
Program Director, SIDS Center of New Jersey; Professor, Department of Pediatrics, Robert Wood Johnson Medical School, New Brunswick, NJ.
Ariana Nunez, MPH
Program Manager, SIDS Center of New Jersey, Robert Wood Johnson Medical School, New Brunswick, NJ
Alissa Sandler, MSW, LCSW
Section Chief, SIDS Center of New Jersey; Clinical Instructor of Pediatrics, RWJMS; Clinical Social Work Supervisor, Joseph M. Sanzari Children's Hospital, Hackensack University Medical Center, Hackensack, NJ.
Lisa Capizzi, MSW, LCSW
Senior, Licensed Clinical Social Worker, SIDS Center of New Jersey, Joseph M. Sanzari Children’s Hospital, Hackensack University Medical Center, Hackensack, NJ.Adjunct Instructor, RWJMS.
Rev. Ann B. Shamy, M.Div
Clergy, Robert Wood Johnson University Hospital, New Brunswick, NJ.
Cathleen Duffy, RNC, MSN, CPNP-PC, CBC
Nurse, Robert Wood Johnson University Hospital, New Brunswick, NJ.
Norma Lewis
Program Assistant, SIDS Center of New Jersey, Robert Wood Johnson Medical School, New Brunswick, NJ. Email: lewisnj@rwjms.rutgers.edu