Parker Health Group Geriatrics Fellowship

We Build Better Doctors.
Join Our Groundbreaking Team.
Our fellowship program in geriatric medicine is built on the strong values of family medicine: comprehensive whole person care that is both patient-centered and patient-directed, within the context of the family and community. We recruit excellent residents with strong medical training, and offer them world-class resources, mentorship, and personalized fellowship experiences. Our graduates are committed to lifelong learning, collaborative partnership, and improvement-based perspectives. While people see so much wrong with healthcare, they see our geriatricians as evidence of what is right. Do you want to be a better doctor?

The Company You'll Keep
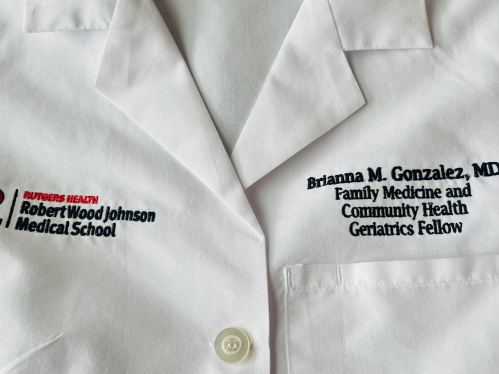
The Parker Health Group (PHG) Geriatrics Fellowship in the PHG Division of Geriatrics at the Department of Family Medicine and Community Health-Robert Wood Johnson Medical School, accredited by the ACGME since 1987, trains skilled and compassionate geriatricians to care for the aging population. We welcome graduates from Family Medicine and Internal Medicine residencies. Fellowship lasts 12 months, with an optional two-year clinical researcher track. Fellows receive training to become effective, efficient, and compassionate geriatricians who will pass their American Board of Family Medicine (ABFM) or American Board of Internal Medicine (ABIM) CAQ examination in Geriatric Medicine and pursue careers managing the complex medical, functional, and emotional needs of our aging population.
The Benefits You'll Accrue
We offer up to 4 Geriatric Fellow positions annually; selected fellows will actively work with our multidisciplinary faculty team, including core family medicine and internal medicine faculty in a multitude of service areas including Inpatient rotations: Geriatrics consultation service; Acute Care; Palliative Care. Outpatient rotations: Subacute Rehab; Long-Term Care; Assisted Living; Adult Daycare; Home-Based Primary Care; Hospice and Palliative Care; and Medical Directorship. Learner-Centered Curriculum with opportunities including: Varied Electives; Research collaboration; Advocacy; Innovation; Leadership; and Additional Outpatient/Inpatient experiences. Geriatric Fellows also have the benefit of the new PHG Center for Longevity as a resource to advance their clinical and leadership skills.
Your Core Geriatrician Faculty
Sara Leonard, MD, FAAFP, Assistant Professor, Department of Family Medicine and Community Health; Director, Geriatrics Fellowship Program; Medical Director, Parker Long-term care, Assisted Living, and Adult Day Programs; Director of Service Innovation, PHG Division of Geriatrics
Fred Kobylarz, MD, MPH, Professor, Department of Family Medicine and Community Health; Medical Director, Parker at Monroe Long-term Care
Joshua J. Raymond, MD, MPH, FAAFP, AGSF, CMD, Professor, Department of Family Medicine and Community Health; Medical Director, Parker at Somerset Post Acute and Long-term Care
David Howarth, MD, MPH, FAAFP, Professor, Department of Family Medicine and Community Health; Geriatrician, Outpatient Services
Educational Curriculum
Fellows participate in outpatient care, comprehensive cognitive assessments, long-term, post-acute and inpatient consultative hospital care. Fellows have rotations in palliative care, wound care, geriatric psychiatry, home based-primary care, hospice/home care, and physical medicine and rehabilitation, along with a wide range of elective rotations and regular collaboration with various specialists and other essential members of the multidisciplinary team.
-
Here’s what you can expect: Ambulatory geriatrics care training combines primary care geriatrics with exposure to relevant complementary ambulatory training experiences. Fellows spend one morning each week performing comprehensive cognitive assessments in our outpatient office in Monroe, NJ, where they also maintain a weekly continuity ambulatory clinic in their core discipline (Family Medicine or Internal Medicine) by seeing a broader age range of patients. Fellows provide outpatient care to residents of Parker at Stonegate (assisted living) and participants in two of Parker’s adult day programs. Additional outpatient experiences are gained through several of the core and elective rotations, which include participation in specialty clinics.
-
Long-term care training is based within three local Parker Homes, which embrace the Eden Alternative model, a person-directed approach that fosters an enriched environment aiming to reduce loneliness, boredom, and helplessness. Fellows provide primary geriatrics care for a panel of patients at these homes under the direct supervision and guidance of faculty geriatricians. Fellows gain administrative skills, medical directorship experience, and familiarity with population health during this time. Additionally, they’re frequently able to maintain continuity with individual patients, for example, by following and caring for them through transitions from assisted living, to post-acute and then long-term care.
-
Inpatient geriatric medicine rotations in acute and consultative geriatric hospital care at the Robert Wood Johnson University Hospital in New Brunswick, NJ, offer ample opportunities for learning within an Age-Friendly Health System. With a medical staff of 1,300 physicians and as the core teaching hospital for the Robert Wood Johnson Medical School, fellows interact with over 300+ residents and fellows from other graduate medical education fields. Fellows work closely with the Family Medicine inpatient service and faculty from the Department of Family Medicine, Department of Medicine, Cancer Institute of New Jersey, and hospital social work, pharmacy, and complementary medicine teams. Fellows provide geriatric consultative care for hospitalized aging individuals and gain hands-on experience in delirium assessments, palliative care consultation and management, decision-making capacity evaluations, and discharge level-of-care determinations.
-
Fellows participate in weekly didactics sessions with learners from Rutgers-New Jersey Medical School in Newark as well as medical students, residents, and pharmacy students from Rutgers New Brunswick. Typically, these sessions include a varied combination of expert speakers, case presentations, journal club, M&M, grand rounds, and formal board review. Additionally, fellows participate in eight half-day didactics sessions through a collaborative with all the Geriatrics Fellowship programs in New Jersey, offering an excellent networking opportunity to fosters collegiality. Fellows are also encouraged to participate in the rich educational offerings available to them as members of the greater Rutgers community.
-
The fellowship curriculum includes a dedicated time for “selective” and “elective” experiences to select areas of clinical interest, explore the state of the art, and develop clinically derived research questions. Time for scholarly activity is woven into fellows’ schedules, allowing them protected time to generate a required scholarly product such as a literature review, abstract, poster, paper or formal presentation. The Research Division of the Department of Family Medicine supports fellows in these activities. In past years fellows have presented posters at national meetings of the American Medical Directors Association and the American Geriatrics Society. Others have co-authored a book chapter or journal article. At the culmination of the fellowship, fellows share their scholarship in a presentation to colleagues and the Parker Health Group community.
-
Fellows are evaluated by fellowship faculty, non-physician staff, and professionals from other disciplines outside of medicine (360 degree evaluations). In turn, fellows provide direct feedback to faculty to improve their learning experiences. We perform milestones evaluations in the middle and at the end of fellowships in accordance with ACGME guidelines. Fellows document their learning with a portfolio of clinical experiences, quality improvement activities, and scholarly products to aid in their future careers.
Salaries and Benefits
The PHG Geriatrics Fellowship offers a PGY-4 salary consistent with those of all graduate medical programs at the medical school. Benefits include enrollment in the desirable NJ State Health Benefits Program, 4 weeks of vacation, 9 Rutgers holidays, 4 personal days, and 12 sick days per academic year, plus a $1,300 educational allowance. The program supports fellows in attending national geriatrics conferences to present their research. Training requires some travel to clinical and didactic venues in central New Jersey. Routine overnight in-hospital call duties are not required.

Contact Us
RWJMS, Department of Family Medicine and Community Health
Parker Health Group Geriatrics Fellowship
Matrix Plaza 1
303 George Street, 6th Floor
New Brunswick, NJ 08901
E-mail: phg-geriatrics@rwjms.rutgers.edu
Program Manager: June Mooney, MPA
Phone: 732-235-7676