
A Publication for Alumni & Friends of Rutgers Robert Wood Johnson Medical School
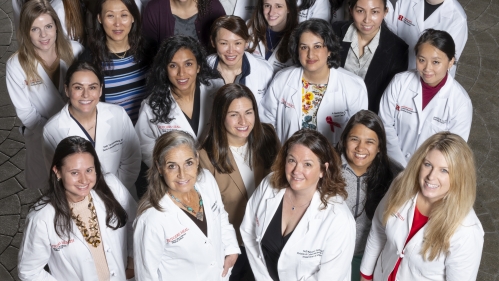
Women in Surgery: Increasing in Numbers—and Influence
Traditionally, surgery has been a male-dominated field. However, gender data both nationally and locally reveals a welcome shift in the specialty.
The most recent data published by the Association of American Medical Colleges (AAMC) revealed that nearly 40 percent of the active physician workforce in the United States comprises women—and many have chosen surgery as their specialty. Nearly a quarter (22.6 percent) of active general surgeons are women, followed by plastic surgery (18 percent), vascular surgery (15 percent), and neurosurgery (10 percent).
“The traditional stereotype is that surgery is male-dominated,” said Leonard Y. Lee, MD, professor and James W. Mackenzie, M.D. Chair of the Department of Surgery at Rutgers Robert Wood Johnson Medical School. “At the national level, white men in particular tend to hold most of the leadership positions for our societies, surgery departments, and even divisions. There are hurdles in terms of changing the culture of these organizations. However, there’s active change ongoing, whether they be local (school or hospital) or national (society), to be more inclusive.”
- Related: Meet Jhillika Patel
The trend is no different at Robert Wood Johnson Medical School, where there are female surgeons in the divisions of vascular surgery, plastic and reconstructive surgery, urology, surgical oncology, and acute care surgery. In fact, there are eight female surgeons each in surgical oncology and acute care surgery.
“Acute care surgery, which used to be called trauma, is often a male-dominated specialty, but in our program, we have equal numbers of women and men,” Dr. Lee noted.
Finding Footing on the Leadership Ladder
The Department of Surgery has been working to promote women into leadership roles and recruit more women to the faculty. When vetting candidates for faculty positions, the Department of Surgery applies an equity lens. A female junior faculty member with specialized diversity, equity, and inclusion training sits on every search committee to inform and guide each decision. Search committees look for the best candidates that fit the medical school’s culture and department’s needs. The application process is blind, so applicants are assessed on their merits and credentials, not gender, race, or other demographics.
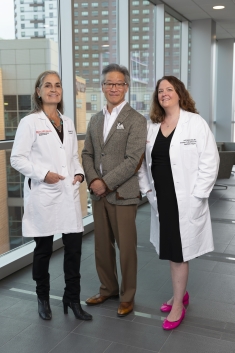
Several female surgeons have risen through the ranks into leadership roles within the department, including Susannah Wise, MD, associate professor of surgery, chief of the Division of General Surgery and vice chair of quality for the Department of Surgery, and colorectal surgeon Nell Maloney Patel, MD, professor of surgery, who recently was promoted to vice chair for education after serving as program director of the general surgery residency. Dr. Maloney Patel also serves as president of the Medical Staff Executive Committee at Robert Wood Johnson University Hospital.
“Many of our women faculty came to the school as junior faculty members at the assistant professor level. I regularly meet with all junior faculty. We talk about how to get promoted, what success looks like for them, and what they’re interested in doing in the world of medicine, whether it’s academics, clinical, etc.,” Dr. Lee said. “As a consequence of those meetings, we’re in the process of promoting seven women to the associate professor level.”
Dr. Wise, the medical school’s first female division chief, chose surgery because it was the nexus of art and science.
“In school, I was interested in the sciences and how people worked but also the fine arts, like painting and figure drawing,” explained Dr. Wise, who specializes in laparoscopic and robotic surgery. “Surgery combined science and mechanics, plus the creative components that made me me. I like that it’s an active profession. We’re asked to make decisions sometimes in a limited timeframe. We have an incredibly intimate connection with our patients.”
Dr. Maloney Patel joined the faculty after graduating from fellowship in 2007. She originally planned to specialize in obstetrics and gynecology, but after her surgical rotation and speaking with a trusted mentor, she switched to surgery.
“I’ve been very lucky. I had good mentors in medical school, so it’s important to me to support other women in surgery,” said Dr. Maloney Patel, who specializes in minimally invasive and robotic surgery.
“I was the first female surgeon named professor here. Nationally, only 21 percent of women make it to associate professor, and then the numbers continue to drop off as leadership increases. I’m proud to have reached that milestone. I’m grateful to the women and men who are my mentors and understand my value to the organization.”
Female Surgeons Shedding Stereotypes
A 2020 report by the Foundation for Narrative Inquiry in Bioethics details female surgeons’ stories of sexual harassment, job discrimination, bullying, intimidation, lack of mentors, and equipment and facilities designed for and dedicated to men, but Drs. Wise and Maloney Patel haven’t experienced this level of disrespect.
“I don’t know any female surgeon who hasn’t experienced some bias due to their gender,” said Dr. Maloney Patel. "Whether it is salary inequity, managing the implicit biases of patients and those around us, or using equipment not made for our sized hands, almost everyone has a story. But the environment is changing as more women enter surgery.”
Regarding interactions with patients, she says patients often benefit from having a female surgeon.
“There’s a growing body of research that shows patients treated by female surgeons have lower rates of postoperative complications than those treated by male surgeons,” Dr. Maloney Patel explained. “Research has found that, in general, patients of female surgeons have lower rates of mortality, readmission and other adverse complications. It is believed that communication style has an impact on these outcomes.”
While patients still often mistake female surgeons for nurses, she makes it a point to introduce herself as the surgeon proactively and explains the role each member of the team has in the patient’s care. Physicians wear badges that say “doctor” to help communicate to patients.
When asked about gender-related bias or discrimination in her life, Dr. Wise said, “It’s not something that has affected me. Everyone is an individual. I’ve never segregated myself as a woman. My gender has never been something I focused on.”
Finding Support for Work Life Balance
When it comes to finding balance while pursuing a demanding career, Dr. Wise said, “Not just women, but everyone has to figure out how to have a life outside their careers. Sometimes, we get so focused on our training that we lose sight of how to make it all work: to have a life, family, and career. You have to make a conscious decision to build the life you want, no matter what field you’re in.”
Dr. Maloney Patel agreed. “Work-life balance is an issue for everyone; it’s not just a women’s issue. Having a life outside of work has been normalized. Residents have kids now, and schools are interested in developing whole people, not just surgeons. One of the most important decisions is choosing the right partner to share the journey with you. I’m fortunate to have a full partner at home in raising our children. He understands my work and the value of it.”
Robert Wood Johnson Medical School is committed to providing a safe and equitable workplace. To help all physicians strike a work-life balance, the medical school offers up to three months of family leave for pregnancy or adoption and six weeks for spouses impacted by family building. The hospital and medical school have breastfeeding and pumping stations to make transitioning back to work more convenient. While there is no formal child care at the hospital or school, Dr. Lee said adding these accommodations is something leadership should consider.
To support women surgeons specifically, the medical school sponsors a local chapter of the Association of Women Surgeons (AWS). This national not-for-profit organization aims to inspire, encourage, and enable aspiring female surgeons to achieve their personal and professional goals. The chapter offers lectures and panel discussions on various topics, including academic leadership, research, family planning, and pay and promotion equality. Through the organization, students are invited to participate in research, mentoring, and shadowing opportunities with attending and resident surgeons.
The university’s OASIS Leadership and Professional Development program also promotes inclusivity by mitigating the isolation and bias that can negatively impact female faculty as they advance through the leadership ladder. Through six months of intensive career development support, faculty can:
- Expand their leadership and communication skills
- Build career-enhancing networks at Rutgers
- Increase scholarly productivity and professional visibility
- Enhance life-work integration and resiliency
- Advance their careers
“There were not a lot of women in urology when I started. You need to consider other ways to find support,” Dr. Maloney Patel advised. “I’ve been lucky to be nominated for leadership opportunities on both the hospital side and the medical school side to allow me to develop as a leader.”
She named L.D. Britt, MD, MPH, former president of the American College of Surgeons and Brickhouse professor of surgery at the Eastern Virginia Medical School, her alma mater, as an influence, as well as Dr. Lee, whose mother was one of the first women doctors in Korea, making him “particularly sensitive to and supportive of women in medicine.” Further, with the school under the direction of a female dean – Amy P. Murtha, MD – Robert Wood Johnson Medical School will continue to be a supportive environment for all physicians, including women in surgery.
“We’ve been fairly successful in recruiting a more diverse faculty,” Dr. Lee said. “If you look at the roster across the Department of Surgery, we’re pretty diverse. And I’m proud of that.”
And, should physicians feel discriminated against or bullied, they are encouraged to report it, he added.
Advice for Future Women in Surgery
For medical students hesitant about the stressors of a career in surgery, Dr. Wise said, “No matter what you do in medicine, you’re going to spend a large majority of your time at work. If you’re concerned about surgery being time-consuming, think about the things that interest you the most and explore those. You’ll be more successful doing something you like.”
“I’m grateful for being able to impact lives in a positive way,” Dr. Maloney Patel added. “Yes, it’s an investment of time and of yourself. You have to love it. I think of it more as a calling. I feel lucky to feel that way.”
Summer Immersion Program Builds Interest in Orthopaedics

When Jhillika Patel (Class of 2026) saw an opportunity to strengthen first-year medical students’ understanding of the field of orthopaedics, she rolled up her sleeves to create a Summer Immersion Program with the Department of Orthopaedic Surgery and the Orthopaedic Surgery Interest Group.
“Recent data shows that more than 69 percent of students decide on pursuing orthopaedics early in their medical school careers,” Patel noted. “Our team wanted to help medical students gain more exposure to orthopaedic subspecialties, learn the day-to-day life in the field, and enable students of all backgrounds to have earlier access to orthopaedics.”
She worked with several mentors to develop the curriculum, including chief resident Jomar Aryee, MD; Brian M. Katt, MD, volunteer faculty; Thomas McPartland, MD, pediatric orthopedic surgeon; and Charles Gatt Jr., MD, associate professor, department chair, and residency director for orthopaedic surgery.
“These physicians have all provided tremendous mentorship and guidance to help figure out the back end of how to implement the program seamlessly,” she said. The program delivers a deeper dive into orthopaedics and includes academic components such as fracture conference, cadaver workshops, and opportunities in the operating room and clinic. Participants also connect with residents and upperclassmen for mentorship.
Four students participated in the 2022 program, and interest has grown each year. In 2023, nine students completed the program, and 11 students in 2024. The program has been recognized by Dean Amy P. Murtha, MD, and has caught the attention of students at medical schools across the country.
“I enjoy seeing the program grow and love to warmly welcome the new interns each year,” Patel said. “From a leadership perspective, there’s always a new challenge to solve every year, which I enjoy tackling as a team. We’re continually looking at how we can make the program better and more efficient for students.”
Early Volunteerism Ignites Interest in Public Health and Medicine
The summer program wasn’t Patel’s first foray into volunteerism. In fact, her interest in becoming a physician began when she joined the American Red Cross’ natural disaster relief and biomedical services efforts. Volunteering post-Hurricane Katrina and later after Hurricane Sandy piqued her interest in public health and medicine. She graduated from Johns Hopkins University with a bachelor’s degree in public health studies and continued her education by earning a master’s degree in biochemistry and molecular biology from the Johns Hopkins Bloomberg School of Public Health.
While in school in Baltimore, Patel spearheaded the development of the Johns Hopkins Bayview Emergency Department (ED) Transitional Volunteering Program under the guidance of the ED vice chief attending physician. Through the program, she connected 35 student volunteers to vulnerable frequent-flyer patients in the Baltimore community to provide access to social services, medication delivery services, and additional support beyond their immediate ED visits. Since 2016, the program has impacted thousands of patients. For her efforts, Patel was recognized with a Volunteer Leadership Award and Provost Undergraduate Research Award from Johns Hopkins University. After graduate school, she conducted orthopaedics clinical research at Brigham & Women’s Hospital/Harvard Medical School before enrolling at Robert Wood Johnson Medical School.
“While at the Brigham, I worked as a research assistant on the shoulder service, learning to manage multicenter trials, design research studies, and work across different teams in a clinical setting. I loved the team environment and am grateful for the experience, as it inspired me to continue integrating research into my career,” Patel explained. “That research sparked my interest in orthopaedic surgery, which I’ve continued exploring in medical school.”
Patel is also passionate about combining her interests in orthopaedic surgery with innovation. She was co-president of the Biomedical Entrepreneurship Network (BEN) and leads the BEN Student Research group. She strives to build a collaborative and supportive environment that fosters students’ creativity in finding new healthcare solutions. In summer 2022, Patel was the only medical student chosen for the Women’s Sports Medicine Summer Internship at the Hospital for Special Surgery in New York City. She shadowed more than 18 women in orthopaedics and the elite athletes they treated, observing surgery, physical therapy, exercise physiology, sports psychology, nutrition, and orthopaedic primary care.
“One of the most fascinating facets of sports medicine is that you’re trying to help a patient get back to maximizing their body’s ability,” Patel said. “It’s clinically complex to treat a sports injury and work with an athlete to ensure they return to play in a way that’s safe long term and maximizes their athleticism. The positive patient-doctor relationships I’ve witnessed and the patients I’ve worked with make me want to help orthopaedic patients achieve better mobility and quality of life and meet their individual goals.”
A Commitment to the Community
Patel’s advice for future medical students is simple: find ways to impact your community.
“Whether it’s the New Brunswick community, your fellow peers, or your hospital system, you can make a significant impact through creative problem-solving,” she explained. “Look for gaps in the healthcare system and then find solutions for solving them. As a medical student, you’re given a unique fund of knowledge; learn how to use it to your advantage, create efficient systems, and get others on board with your ideas to take action in your community.”
Several organizations have recognized Patel’s commitment to the orthopaedics community. For her work developing the Summer Immersion Program and her research accomplishments, she earned a scholarship from the Ruth Jackson Orthopaedic Society to attend the American Academy of Orthopedic Surgeons’ 2024 Annual Meeting. She also received the New Jersey State Governor’s Volunteerism Award in the Healthcare Service category from Gov. Phil Murphy for volunteering with the American Red Cross.
“I’m grateful for the support while developing these new programs from the ground up. I love the challenge. My goal is always to make sustainable programs that positively impact systems,” Patel said. “It’s been a privilege connecting with so many mentors, forging new teams with my peers, and helping drive these programs to benefit students. In the future, I want to continue giving back whenever possible.”
