
About the Department of Orthopaedic Surgery
About
The mission of the Department of Orthopaedic Surgery has three main arms. They are:
- to offer excellent care to all the patients we serve,
- to provide superb clinical and academic education and training to its residents,
- and to advance the field of orthopaedic surgery through contributions to research.
For nearly a half a century, the department has been continuously making strides towards these goals. We boast the premiere site for orthopaedic training in the state of New Jersey, and the diverse paths that our residents take are a testament to the breadth and depth of training they receive here. The faculty at Robert Wood represent a healthy mix of talented physicians trained all over the country, as well as at Robert Wood Johnson. The diversity in their training serves to amplify the training experience our residents receive.
Message from the Chair

The Orthopaedic Surgery Residency Program at Robert Wood Johnson Medical School is devoted to producing honest and ethical surgeons with excellent credentials for teaching, service and research. Our superb, privademic teaching staff, has been instrumental in accomplishing this goal. The confluence of a high volume and breadth of surgical cases, with an excellent clinical office experience results in an extremely comprehensive education for our trainees.
Working at a Level 1 trauma center and working with NCAA Division 1 athletic programs provides a tremendous experience for the residents. Our busy pediatric orthopaedic service provides exposure to this population during all five years of residency training. The suburban location of Robert Wood Johnson Medical School and its affiliate teaching institution St. Peter’s University Hospital provide an environment that satisfies the varied cultural, athletic and educational needs for a strong foundational education in orthopaedic surgery.
Charles Gatt, MD
Chair, Department of Orthopaedic Surgery
Mission
In the Department of Orthopedic Surgery at Robert Wood Johnson Medical School, our goals are to teach clinical knowledge, demonstrate the surgical technique, and provide academic opportunities that will allow our trainees to competently and ethically practice as an academic or community leader, and make meaningful contributions to the field of Orthopaedic Surgery.
We accomplish these goals through trainee exposure to a wide variety of clinical settings from seeing patients at Robert Wood Johnson’s Level 1 Trauma Center to providing care for athletes in the NCAA’s Big 10, as well as by endorsing a host of scholarly activities including opportunities to be involved in basic science and clinical research, to teach other trainees and medical students, and to travel to local and national conferences to learn from experts in the field.
Events
Residency
Orthopaedic Residency Program
The Department of Orthopaedic Surgery offers three residency positions per year. Applicants are selected through the National Resident Matching Program. The program is five years and includes comprehensive training in adult and pediatric orthopaedics as specified by the American Board of Orthopaedic Surgery.
Orthopaedic Surgery Interest Group (OSIG)
The OSIG is a student-led organization that aims to:
- Provide exposure to orthopedic specialties, including hands-on workshops, observation and participation in clinical settings, and introductions to specific subspecialties
- Establish long-lasting mentorship relationships
- Provide research and presentation opportunities
- Build on previous OSIG E-Boards’ efforts to expand diversity in orthopedic specialties
- Foster relationships between medical students interested in orthopedic surgery
We achieve these goals by hosting lectures, panels, and hands-on skills workshops, coordinating operative and non-operative shadowing opportunities, organizing social events to connect students, residents, and alumni, and by offering involvement in research projects.










2024 Orthopaedic Match Celebration Brunch
Medical Student Orthopaedic Surgery Research Symposium
Women In Orthopaedics Panel
Women In Orthopaedics Panel
2024 Orthopaedic Match Celebration
2024 OSIG E-Board and faculty advisor Dr. Brian Katt
OSIG Annual Highland Park 5K
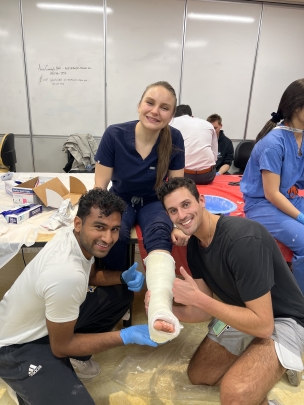
Casting and Splinting Workshop
OSIG and RJOS Mixer
RPM1000 Workshop
Suturing Workshop
Accordion Content
-
In line with our mission to foster camaraderie among students interested in orthopaedics, OSIG hosts student-only panels to facilitate the exchange of experiences between students of all classes and educational faculty-student panels.
A few examples include the M2 Panel on M1 Summer Experiences, during which upperclassmen share their experiences in various summer programs with first-year students, helping them find suitable opportunities. The Research Year Fellowship Panel provides insights into the pros and cons of taking a research year from RWJMS and NJMS students who had either taken a research year or opted not to. The Annual M4 Post-Match Panel features graduating students dissecting the residency application process, current year’s Match statistics, and providing advice on matching into orthopaedics. To introduce students to various sub-specialties in orthopaedics, OSIG invites operative and non-operative physicians along with physical therapists to speak about their career paths, and the benefits and challenges of their field. Our Fall Women In Ortho Panel brings women orthopaedic surgeons from Rutgers and other institutions to campus for a networking dinner with students.
-
Throughout the semester, OSIG hosts a multitude of bioskills workshops, including suture workshops, cadaver and sawbones workshops with companies like Stryker, and b-One splinting/casting labs as well a virtual reality surgical simulation with Osso VR! In Spring 2024, OSIG hosted its inaugural Orthopaedic Trauma Simulation Workshop. Held at the Rutgers Pharmacy School Simulation Lab, the Trauma workshop offered a unique interactive experience where students rotated through four stations, learning about trauma case management, injury anatomy, stabilization and splinting, reading X-rays, and more.
-
To meet the demand for student research projects, our Chair of Research manages a database of current research projects and connects students with academic surgeons at RWJ, NJMS, and Monmouth Medical Center. Our students involved in scholarship are invited to participate in the Department of Orthopaedics Research Update and the Summer Orthopaedics Research Day presentation and poster sessions.
-
Throughout the academic year, OSIG manages a robust shadowing program with weekly OR shadowing opportunities across various subspecialties at RWJUH and SPUH and weekly clinic shadowing spots at RWJUH, SPUH, and RWJ Pediatric Orthopaedics. OR shadowing days allow students to experience a “day in the life of a resident” starting with morning rounds at 5:30 am continuing to education sessions and finally observing surgical cases.
-
OSIG facilitates two summer immersion programs. The RWJ Orthopaedic Summer Immersion program provides RWJMS and outside students with a week-long experience for rising M2s interested in pursuing orthopaedic surgery. During this experience-filled week, two cohorts of students shadow attendings and residents in both clinic and the operating room across various sub-specialties. Program participants attend educational activities such as fracture conferences and grand rounds as well as journal clubs, industry workshops, and networking dinners.
The second formal immersion program is the Orthopaedic Surgery Bootcamp for rising M4 students applying into Orthopaedic Surgery Residency Programs. This week-long session provides students with the necessary skills to succeed in sub-iInternships and away rotations, which are imperative to successfully match in a field like orthopaedics.
-
By regularly participating in OSIG events and orthopaedic shadowing, students can earn a Non-Credit Elective (NCE) notation on their transcript during their preclinical years. To qualify for the NCE, students must attend a total of eight lectures or events throughout their MS1-MS2 years and complete a minimum of 12 shadowing hours through the OSIG shadowing program. This can be done in various settings, including clinics, the OR, on-call shifts, or private physician offices.
Medical Student Rotations
THIRD YEAR MEDICAL STUDENTS
Third year medical students have the opportunity to rotate through orthopedics as part of their surgery rotation. We encourage students to spend additional time with us as fourth year students if they are interested in pursuing an orthopedic residency or have interest in the musculoskeletal system.
During their third year, medical students will have the opportunity to learn the basics of the physical exam of the extremities, observe fracture care in the emergency room, participate in seeing patients in the outpatient clinics, and observe surgery in the operating room. At the end of the rotation, all students should be able to perform a basic musculoskeletal exam, and to be comfortable with the terminology involved in describing fractures as seen on x-ray.
FOURTH YEAR MEDICAL STUDENTS
Fourth year medical students are invited to spend 2-4 weeks working on the orthopedic services at Robert Wood Johnson University Hospital and St. Peter’s University Hospital. Students spend approximately 70% of the rotation in the hospital and 30% in the outpatient offices with full-time and volunteer faculty. Emphasis is placed on physical exam, applied anatomy, and basic clinical decision making. Students have the choice of rotating on the Trauma, Adult Reconstruction, Pediatric, Sports, and Hand services.
Student responsibilities include attending daily morning rounds and all conferences. Active participation in all clinical and operative procedures is encouraged. At the conclusion of the rotation, students will give a 10 minute presentation on an interesting case or germane topic selected by the student. Taking night call to gain a better understanding of resident on-call responsibilities is a required part of the 4th year experience. This opportunity also allows the student to spend one-on-one time with the on call resident. In the past, students performing well during their visiting rotation have been given strong consideration during the residency application process.
Robert Wood Johnson University Hospital

State-of-the-Art Clinical Settings
Learn in dynamic environments where medical education, leading-edge research, and outstanding patient care converge. Our principal teaching hospital, Robert Wood Johnson University Hospital, and clinical affiliations with RWJBarnabas Health and numerous hospitals and ambulatory care sites across New Jersey provide extraordinary opportunities to hone your skills under the guidance of renowned mentors and clinicians.
Life at Rutgers

Envision Yourself Here
Rutgers is located in central New Jersey in the city of New Brunswick and across the Raritan River in Piscataway. Middlesex-Somerset-Hunterdon counties rank fourth in per capita income nationwide. It is a manufacturing center, agricultural center, high-tech corporate center, and small-town America rolled into one.
Who We Are
Departmental teaching responsibilities are distributed among the full-time faculty with assistance provided by a large number of private faculty. Over 40 orthopaedic surgeons are directly involved in the education of the orthopaedic residents. Clinical instruction in the operating room is carried out on a one-to-one basis. Emphasis is placed on level appropriate independent decision making and development of operative skills.
Faculty didactic lectures are conducted on a fixed schedule. A multitude of academic conferences cover all orthopaedic sub-specialties. A two year didactic lecture cycle on core topics in orthopedics is conducted during protected academic time one half day per week. An emphasis is placed on current primary literature and board review.
Accordion Content
-
- Cristobal Beiro, MD
- Patrick S. Buckley, MD
- Charles J. Gatt, Jr., MD
- Heather Harnly, MD
- Shawn Sieler, MD
- Kenneth G. Swan, MD
- Eric Nussbaum, MEd, ATC, LAT
-
- Mark S. Butler, MD
- Justin Fleming, DPM, FACFAS
-
- Deidre Bielicka, MD
- Brian M. Katt, MD
- David Kirschenbaum, MD
- Timothy Leddy, MD
- Lewis Levine, MD
- James T. Monica, MD
- Michael Lu, MD
-
- Gino Chiappetta, MD
- Richard Klein, MD
- Matthew McDonnell, MD
-
- Mark S. Butler, MD
- David R. Polonet, MD
- Sergei Pushilin, MD
- Carlos A. Sagebien, MD
-
- William Baione, MD
- David A. Harwood, MD
- Stephen Kayiaros, MD
Overview
Research is an integral part of each resident's experience at Robert Wood Johnson Medical School. The ACGME requires that each resident produce at least one publishable research project during their 5 years of residency. Currently there are multiple IRB approved clinical prospective and retrospective studies being performed being performed at Robert Wood Johnson University Hospital. All research is driven by the residents with guidance from attending faculty. Residents are required to present their research updates on a quarterly basis to the department, as well as at the RWJ Orthopaedic Research Symposium held at the end of the academic year.
The Orthopaedic Residency Program is also intimately involved with a musculoskeletal biomechanics laboratory chaired by Dr. Dunn located within Robert Wood Johnson University Hospital. This laboratory performs basic science research and provides an opportunity for orthopaedic residents to become involved in tissue engineering as well as the ability to perform animal and cadaveric science research.
For more information regarding ongoing research, or information about becoming involved with orthopaedic research at Robert Wood Johnson Medical School, please contact Dr. Gatt or Barbara Perry.
Orthopaedic Research Laboratory
Our laboratory specializes in the tissue engineering and biomechanics of orthopedic soft tissues including:
- Ligaments and tendons
- Menisci
- Joint surfaces
- Intervertebral disc
Our current projects include:
- Protective treatments to allow for ionizing radiation sterilization of musculoskeletal soft tissue allografts
- Development of a hybrid polymer fiber / collagen sponge for meniscus tissue engineering
- Development of a hybrid scaffold for intervertebral disc tissue engineering
- Understanding of meniscal root mechanics and testing of various fixation methods
Lab Research
Orthopedic injuries are extremely common, especially to the knee. However, the avascular nature of the synovial areas makes it extremely difficult for injured soft tissues to regenerate. Failure to treat these injuries can lead to injury of other soft tissues, leading to cartilage degeneration and improper weight loading. These can cause a patient pain and discomfort, creating a need for tissue engineering of orthopedic tissues. Specifically, we focus on ligament, meniscus, and articular cartilage tissue engineering.
Anterior Cruciate Ligament
Previous work has aimed at creating a scaffold for tissue engineering of the ACL. Material sources include biological (bovine dermal collagen, Bombyx Mori silk) and synthetic (PLLA, poly DTDDD) polymers. Currently, efforts are aimed towards developing an effective radioprotection treatment of tendon allografts to combat the decrease in mechanical integrity following sterilization.
Mensicus
Currently, we are working on a hybrid polymer (poly DTDDD) fiber/collagen sponge scaffold for meniscus TE. Weaving fibers into the pattern to the right can provide sufficient mechanical integrity, both radially and circumferentially, whereas the collagen sponge adds biocompatibility and bioactivity. The polymer degrades over time, giving way to natural tissue, and the collagen sponge is remodeled to form a natural, functional extracellular matrix. Future studies will also experiment with PLLA polymer, as well as partial mensicus implants.
Who We Are
The Orthopaedic Research Laboratory is under the direction of Michael Dunn, PhD, and Charles Gatt Jr, MD. There are currently two graduate students from the Department of Biomedical Engineering at Rutgers University. Additionally, medical students may choose the Orthopaedic Research Laboratory as a site for a four-week research elective. Lastly, we would like to acknowledge the vivarium staff headed by Barbara Perry, and administrative staff headed by Michelle Allen.
In addition to the research done in this lab, many of its members have participated together in extracurricular activities, most notably intramural sports at Rutgers University. These have included volleyball and softball.
Accordion Content
-
Michael Dunn, PhD
Director
dunnmg@rwjms.rutgers.eduMichael Dunn received his BS in Biomedical Engineering from Boston University in 1981. He then completed his graduate work at Rutgers University (MS1983, PhD 1987) under the direction of Dr. Fred Silver. He has been the director of the Orthopaedic Research Laboratory since and is currently an Associate Professor of Orthopaedic Surgery at Robert Wood Johnson Medical School and Graduate Faculty Member for the Robert Wood Johnson Medical School Program in Biomedical Engineering.
Dunn’s personal interests include baseball, basketball, and golf, and he likes to watch almost any sport. He is an avid New York Yankees and New York Giants fan.
Charles Gatt, MD
Associate Professor
Residency Director, Orthopaedic Surgery
allenmi@rwjms.rutgers.eduCharles Gatt obtained his B.S. in Chemical Engineering from Lafayette College in Easton, PA in 1985, and obtained his MD in 1989 from the UMDNJ Robert Wood Johnson Medical School. After his Orthopaedic Surgery residency at UMDNJ in 1994, and a one-year Orthopaedic Sports Medicine Fellowship at the Cleveland Clinic, Gatt began practicing as an orthopaedic surgeon, and is currently an Associate Professor, and residency director, of Orthopaedic Surgery at Robert Wood Johnson Medical School. A few of Gatt’s honors and additional publications are shown below.
- Herodicus Award - Best Resident Paper at AOSSM, Sun Valley, Idaho (1993)
- Preceptor of the Year, Glendale Adventist Department of Family Practice (1997)
- Alpha Omega Alpha Honor Society (1999)
- Department of Surgery Volunteer Faculty Award (2001)
Sarvazyan A, Tatarinov A, Egorov V, Airapetian S, Kurtenok V, Gatt CJ Jr. (2009) Application of the dual-frequency ultrasonometer for osteoporosis detection. Ultrasonics. 49(3):331-337.
Aronowitz ER, Parker RD, Gatt CJ (2001) Arthroscopic identification of the popliteofibular ligament. Arthroscopy. 17(9):932-939.
Gatt CJ Jr., Hosea TM, Palumbo RC, Zawadsky JP (1997) Impact loading of the lumbar spine during football blocking. Am. J. Sports. Med. 25(3):317-321.
Hosea TM, Gatt CJ Jr. (1996) Back pain in golf. Clin. Sports. Med. 15(1):37-53.
-
Kholoud Baste
Kholoud grew up in the Chicago area and has a B.S. in Biomedical Engineering from the University of Illinois at Chicago. Outside of the lab, Kholoud spends her time rock climbing and baking various deserts.Matteau Bonner
Mattheau grew up in Mississauga, Ontario, Canada. After obtaining a B.S. in Biomedical Engineering while being a NCAA D1 swimmer at NJIT in Newark, NJ in the spring of '21, Matt began his PhD journey at Rutgers in the fall of '21. Outside of the lab, Matt enjoys Y2K videography, trips to NYC, basketball, and Formula 1. He is also a huge Toronto Raptors fan. -
Gnaneswar Chundi
Gnaneswar grew up in Edison, New Jersey. He is currently working on a BS in Biomedical Engineering and Computer Science at Rutgers University. Outside of the lab, Gnaneswar enjoys playing tennis and is part of the Rutgers club team. He is a big NBA and NFL fan and supports the Cleveland Cavaliers and Cleveland Browns. He also plays the cello and works as an EMT.Jasmine Berrios
Jasmine is currently pursuing a Bachelor's degree in Exercise Science at Rutgers University, New Brunswick. Her interest in orthopedics stems from her own personal sport injury experiences, which have fueled her desire to be a part of innovative orthopedic research. Outside of the lab, she enjoys painting and swimming when her schedule permits. She is also a proud Rutgers football and basketball supporter as well as a Yankees and Seahawks fan.Bowie Shreiber
Bowie is a junior at Duke University pursuing a BSE in biomedical engineering. His research interests include tissue and molecular engineering and biomechanics. -
- William Pfaff, PhD
- Salim Ghodhbane, PhD
- Jay Patel, PhD
- Aaron Merriam, PhD
- Justin Rice
- Grace Bundens, PhD
- Aaron Seto, PhD
- Eric Balint, PhD
- Eleni Panas, PhD
- Nick Tovar, PhD
- Andrea Caruso, PhD
- Jordan Katz, PhD
- Jeffrey Cartmell, PhD
Publications
Accordion Content
-
Recent Clinical Studies
- Aryee JNA, Frias GC, Haddad DK, et al. Understanding Variations in the Management of Displaced Distal Radius Fractures With Satisfactory Reduction. Hand (N Y). Published online March 8, 2024. doi:10.1177/15589447241233709.
- Tawfik AM, Elkhechen JN, Aryee J, Sirch F, Filtes P, Katt BM. The Effect of Thumb Carpometacarpal Joint Corticosteroid Injections on Outcomes Following Arthroplasty. Hand (N Y). 2023;18(7):1142-1147. doi:10.1177/15589447221081862.
- Alter TH, Noh KJ, Monica JT. Management of Isolated Ulnar Shaft Fractures. JBJS Rev. 2023;11(6):e22.00254. Published 2023 Jun 5. doi:10.2106/JBJS.RVW.22.00254.
- Chan PYW, Silver JM, Phelan J, Moore K, Green A, Katt B. How Are Radial Height and Radial Shortening Defined in the Treatment of Distal Radius Fractures? A Critical Review. Hand (N Y). Published online January 24, 2023. doi:10.1177/15589447221150506.
- Alter TH, Romeo PV, Bielicka DL, Monica JT. Distal Intersection Syndrome Between Second and Third Dorsal Compartments of the Wrist. Cureus. 2023;15(3):e36919. Published 2023 Mar 30. doi:10.7759/cureus.36919.
- Aryee JNA, Silver JM, Grossman J, Polonet D, Buckley PS. Acute Exertional Bilateral Thigh Compartment Syndrome in a Patient with Rhabdomyolysis After Spin Class: A Case Report. JBJS Case Connect. 2023;13(2):e23.00030. Published 2023 Jun 15. doi:10.2106/JBJS.CC.23.00030.
- Toci GR, Green A, Mubin N, et al. Patient Adherence With At-Home Hand and Wrist Exercises: A Randomized Controlled Trial of Video Versus Handout Format. Hand (N Y). 2023;18(4):680-685. doi:10.1177/15589447211052750.
- Alter TH, Varghese BB, DelPrete CR, Katt BM, Monica JT. Reduction Techniques in Volar Locking Plate Fixation of Distal Radius Fractures. Tech Hand Up Extrem Surg. 2022;26(3):168-177. Published 2022 Sep 1. doi:10.1097/BTH.0000000000000380.
- Avendano JP, Gallagher DO, Hawes JD, et al. Interfacing With the Electronic Health Record (EHR): A Comparative Review of Modes of Documentation. Cureus. 2022;14(6):e26330. Published 2022 Jun 25. doi:10.7759/cureus.26330.
- Alter TH, Helbig T, Chiappetta G. Case report: Multiple sclerosis diagnosis after anterior lumbar interbody fusion and presumed COVID-19 infection. Surg Neurol Int. 2022;13:125. Published 2022 Mar 31. doi:10.25259/SNI_192_2022.
- Katt BM, Tawfik AM, Aryee J, Aita D, Beredjiklian PK, Fletcher D. The Efficacy of Intra-Articular Versus Extra-Articular Corticosteroid Injections in the Thumb Carpometacarpal Joint. J Hand Surg Glob Online. 2022;4(3):128-134. Published 2022 Feb 11. doi:10.1016/j.jhsg.2022.01.002.
- Green AH, Forlizzi JM, Boyle J, et al. Estimating the Nosocomial Transmission Rate of COVID-19 in Orthopaedic Surgery Patients During the Peak of the Pandemic. Orthop Res Rev. 2022;14:215-224. Published 2022 Jun 18. doi:10.2147/ORR.S361116.
- Mennona S, Mascarenhas D, Green A, et al. Novel Method for Reduction of Distal Radius Fractures. J Orthop Trauma. 2021;35(Suppl 2):S20-S21. doi:10.1097/BOT.0000000000002179.
- Coyle RM, Tawfik AM, Green A, Katt BM, Glickel SZ. Coding Practices in Hand Surgery and Their Relationship to Surgeon Compensation Structure. J Hand Surg Glob Online. 2021;3(4):161-166. Published 2021 May 26. doi:10.1016/j.jhsg.2021.04.004.
- Tawfik AM, Silver JM, Katt BM, Patankar A, Rivlin M, Beredjiklian PK. Patient Perceptions of COVID-19 Precautions and Their Effects on Experiences With Hand Surgery. J Hand Surg Glob Online. 2021;3(4):167-171. doi:10.1016/j.jhsg.2021.04.003.
Recent Basic Science Studies
- Ryan J, Imbergamo C, Sudah S, Kirchner G, Greenberg P, Monica J, Gatt C. Platelet-Rich Product Supplementation in Rotator Cuff Repair Reduces Retear Rates and Improves Clinical Outcomes: A Meta-analysis of Randomized Controlled Trials. Arthroscopy. 2021 Aug;37(8):2608-2624. doi: 10.1016/j.arthro.2021.03.010. Epub 2021 Mar 17. PMID: 33744318; PMCID: PMC8349828.
- Bateman DK, Preston JS, Kayiaros S, Tria AJ Jr. Synthetic Mesh Allograft Reconstruction for Extensor Mechanism Insufficiency After Knee Arthroplasty. Orthopedics. 2019 Jul 1;42(4):e385-e390. doi: 10.3928/01477447-20190403-02. Epub 2019 Apr 9. PMID: 30964536.
- Patel JM, PhD , Brzezinski A, MD , Raole DA, MBS , Dunn MG, PhD , Gatt CJ, Jr, MD (2018) "Interference Screw Versus Suture Endobutton Fixation of a Fiber-Reinforced Meniscus Replacement Device in a Human Cadaveric Knee Model". Am J Sports Med. Vol 46, Issue 9, pp. 2133 - 2141. doi: 10.1177/0363546518773737 May 30, 2018.
- Brzezinski A, Ghodbane SA*, Patel JM*, Perry BA, Gatt CJ, Dunn MG (2017) “The Ovine Model for Meniscus Tissue Engineering: Considerations of Anatomy, Function, Implantation, and Evaluation”. Tissue Eng Part C Methods. 2017 Dec; 23(12):829-841 doi: 10.1089/ten.TEC.2017.0192. Epub 2017 Sep 29.
- Complications Associated with Intra-Articular and Extra-Articular Corticosteroid Injections. Honcharuk E, Monica J. JBJS Rev. 2016 Dec 13;4(12). pii: 01874474-201612000-00002. doi: 10.2106/JBJS.RVW.16.00004.
-
- Ekwueme EC, Patel JM, Freeman JW, Danti S. “Applications of Bioresorbable Polymers in the Skeletal Systems (Cartilages, Tendons, Bones).” Bioresorbable Polymers for Biomedical Applications: From Fundamentals to Translational Medicine. 2017, ISBN:9780081002667. pp391-422.
- Dunn MG (2006) Tissue engineering strategies for ACL regeneration. In Walsh WR, editor. Repair and regeneration of ligaments, tendon, and joint capsule. Humana Press. pp 279-296.
- Gertzman AA, Sunwoo MH, Raushi D, Dunn M (2005) The effect of cold gamma radiation sterilization on the properties of demineralized bone matrix. In Kennedy JF, Phillips GO, Williams PA, editors. Sterilization of tissues using ionizing radiations. CRC Press. pp 151-161.
- Dunn MG (1995) Biomechanics of ligament reconstruction. In Tria AJ, editor. Ligaments of the knee. Churchill Livingstone. pp 275-286.
-
- Patel, J. M., Brzezinski, A., Ghodbane, S. A., Tarapore, R., Lu, T. M., Gatt, C. J., and Dunn, M. G. "Personalized Fiber-Reinforcement Networks for Meniscus Reconstruction." ASME. J Biomech Eng. May 2020; 142(5): 051008. https://doi.org/10.1115/1.4045402
- Ghodbane, SA, Patel, JM, Brzezinski, A, Lu, TM, Gatt, CJ, Dunn, MG. Biomechanical characterization of a novel collagen-hyaluronan infused 3D-printed polymeric device for partial meniscus replacement. J Biomed Mater Res Part B. 2019: 107B: 2457– 2465.
- Ghodbane, Salim & Murthy, N. Sanjeeva & Dunn, Michael & Kohn, Joachim. (2019). Achieving molecular orientation in thermally extruded 3D printed objects. Biofabrication. 11. 10.1088/1758-5090/ab1d44.
- Salim Ghodbane, Andrzej Brzezinski, Jay Patel, William H. Plaff, Kristen N. Marzano, Charles J. Gatt, and Michael G. Dunn. Partial Meniscus Replacement with a Collagen-Hyaluronan Infused Three-Dimensional Printed Polymeric Scaffold. Tissue Eng Part A. 2019;25(5-6):379-389. doi:10.1089/ten.TEA.2018.0160
- Patel, J. M., Brzezinski, A., Raole, D. A., Dunn, M. G., & Gatt, C. J. (2018). Interference Screw Versus Suture Endobutton Fixation of a Fiber-Reinforced Meniscus Replacement Device in a Human Cadaveric Knee Model. The American Journal of Sports Medicine, 46(9), 2133–2141. https://doi.org/10.1177/0363546518773737
- Patel JM, Brzezinski A, Raole DA, Dunn MG, Gatt CJ (2017) Interference screw versus suture endobutton fixation of a fiber-reinforced meniscus device. Am J Sports Med. (in preparation).
- Patel JM, Ghodbane SA, Brzezinski A, Gatt CJ, Dunn MG (2017) Tissue-engineered meniscal replacement using a fiber-reinforced total meniscus scaffold in a two-year ovine model. Am J Sports Med. Submitted.
- Patel JM, Jackson RC, Schneider GL, Ghodbane SA, Dunn MG (2017) Carbodiimide cross-linking counteracts the detrimental effects of gamma irradiation on the physical properties of collagen-hyaluronan sponges. J Mech Behav Biomed Mater. In Revision.
- Patel JM, Dunn MG, Gatt CJ. “System and method for making personalized fibrocartilage implants.” International PCT Application No. WO2017095662 A1. June 8, 2017.
- Brzezinski A*, Ghodbane SA*, Patel JM*, Perry BA, Gatt CJ, Dunn MG (2017) The Ovine Model for Meniscus Tissue Engineering: Considerations of Anatomy, Function, Implantation, and Evaluation. Tissue Eng Part C. Accepted.
- Patel JM, Merriam AR, Kohn J, Gatt CJ, Dunn MG (2016) Negative Outcomes of Poly(l-Lactic Acid)Fiber-Reinforced Scaffolds in an Ovine Total Meniscus Replacement Model. Tissue Eng Part A. 22(17-18):1116-1125.
- Patel JM, Merriam AR, Culp BM, Gatt CJ, Dunn MG (2016) One-year Outcomes of Total Meniscus Reconstruction Using a Novel Fiber-Reinforced Scaffold in an Ovine Model. Am J Sports Med. 44(4):898-907.
- Patel JM, Brzezinski A, Lu T, Tarapore R, Dunn MG, Gatt CJ. “Contact Stress Profile of a Fiber-Reinforced Total Meniscus Replacement Device”, Paper Presentation, Orthopaedic Research Society Annual Meeting. San Diego CA. March 2017.
- Patel JM, Ghodbane SA, Gatt CJ, Dunn MG. “ER-14 Development of Novel Medical Devices to Restore Knee Function and Prevent Osteoarthritis”, Poster and Podium Presentation. Armed Forces Institute of Regenerative Medicine II Investigators Meeting. Bethesda MD. Jan 2017.
- Schneider G, Patel JM, Dunn MG. “Platelet Rich Plasma: Isolation and Potential Application in an Ovine Model”, Poster,American Medical Association Medical Student Section Interim Meeting. Orlando FL. Nov 2016.
- Brzezinski A, Patel JM, Lu T, Tarapore R, Dunn MG, Gatt CJ. “Load-Sharing Properties of a Fiber-Reinforced Meniscus Scaffold”, Poster, New Jersey Symposium on Biomaterials Science. Iselin NJ. Oct 2016.
- Patel JM, Gatt CJ, Dunn MG. “Preclinical Development and Testing of a Fiber-Reinforced Total Meniscus Replacement Device”, Poster, Gordon Research Conference: Musculoskeletal Biology and Bioengineering. Andover NH. August 2016.
- Panas-Perez E, Gatt CJ, Dunn MG (2012) Development of a silk and collagen fiber scaffold for anterior cruciate ligament reconstruction. J. Mater. Sci. Mater. Med. Epub.
- Seto AU, Gatt CJ Jr., Dunn MG (2012) Sterilization of tendon allografts: a method to improve strength and stability after exposure to 50 kGy gamma radiation. Cell Tissue Bank. Epub.
- Balint E, Gatt CJ Jr., Dunn MG (2012) Design and mechanical evaluation of a novel fiber-reinforced scaffold for meniscus replacement. J. Biomed. Mater. Res. A. 100(1):195-202.
- Tovar N, Bourke S, Jaffe M, Murthy NS, Kohn J, Gatt C, Dunn MG (2010) A comparison of degradable synthetic polymer fibers for anterior cruciate ligament reconstruction. J. Biomed. Mater. Res. A. 93(2):738-747.
- Seto A, Gatt CJ Jr., Dunn MG (2009) Improved tendon radioprotection by combined cross-linking and free radical scavenging. Clin. Orthop. Relat. Res. 467(11):2994-3001.
- Seto A, Gatt CJ Jr., Dunn MG (2008) Radioprotection of tendon tissue via crosslinking and free radical scavenging. Clin. Orthop. Relat. Res. 466(8):1788-1795.
- Caruso AB, Dunn MG (2005) Changes in mechanical properties and cellularity during long-term culture of collagen fiber ACL reconstruction scaffolds. J. Biomed. Mater. Res. A. 74(4):388-397.
- DePaula CA, Truncale KG, Gertzman AA, Sunwoo MH, Dunn MG (2005) Effects of hydrogen peroxide cleaning procedures on bone graft osteoinductivity and mechanical properties. Cell Tissue Bank. 6(4):287-298. (PDF)
- Katz JM, Roth CM, Dunn MG (2005) Factors that influence transgene expression and cell viability on DNA-PEI-seeded collagen films. Tissue. Eng. 11(9-10):1398-1406.
- Bourke SL, Kohn J, Dunn MG (2004) Preliminary development of a novel resorbable synthetic polymer fiber scaffold for anterior cruciate ligament reconstruction. Tissue. Eng. 10(1-2):43-52.
- Cartmell JS, Dunn MG (2004) Development of cell-seeded patellar tendon allografts for anterior cruciate ligament reconstruction. 10(7-8):1065-1075.
- Caruso AB, Dunn MG (2004) Functional evaluation of collagen fiber scaffolds for ACL reconstruction: cyclic loading in proteolytic enzyme solutions. J. Biomed. Mater. Res. A. 69(1):164-171.
- Ohan MP, Dunn MG (2003) Glucose stabilizes collagen sterilized with gamma irradiation. J. Biomed. Mater. Res. A. 67(4):1188-1195.
- Ohan MP, Weadock KS, Dunn MG (2002) Synergistic effects of glucose and ultraviolet irradiation on the physical properties of collagen. J. Biomed. Mater. Res. 60(3):384-391.
- Talbott SM, Cifuentes M, Dunn MG, Shapses SA (2001) Energy restriction reduces bone density and biomechanical properties in aged female rats. J. Nutr. 131(9):2382-2387.
- Cartmell JS, Dunn MG (2000) Effect of chemical treatments on tendon cellularity and mechanical properties. J. Biomed. Mater. Res. 49(1):134-140.
- Bellincampi LD, Closkey RF, Prasad R, Zawadsky JP, Dunn MG (1998) Viability of fibroblast-seeded ligament analogs after autogenous implantation. J. Orthop. Res. 16(4):414-420.
- Bellincampi LD, Dunn MG (1997) Effect of crosslinking method on collagen fiber-fibroblast interactions. J. Appl. Polym. Sci. 63:1493-1498.
- Dunn MG, Bellincampi LD, Tria AJ, Zawadsky JP (1997) Preliminary development of a collagen-PLA composite for ACL reconstruction. J. Appl. Polym. Sci. 63:1423-1428.
- Weadock KS, Miller EJ, Keuffel EL, Dunn MG (1996) Effect of physical crosslinking methods on collagen-fiber durability in proteolytic solutions. J. Biomed. Mater. Res. 32(2):221-226.
- Dunn MG, Liesch JB, Tiku ML, Zawadsky JP (1995) Development of fibroblast-seeded ligament analogs for ACL reconstruction. J. Biomed. Mater. Res. 29(11):1363-1371.
- Weadock KS, Miller EJ, Bellincampi LD, Zawadsky JP, Dunn MG (1995) Physical crosslinking of collagen fibers: comparison of ultraviolet irradiation and dehydrothermal treatment. J. Biomed. Mater. Res. 29(11):1373-1379.
- Dunn MG, Maxian SH, Zawadsky JP (1994) Intraosseous incorporation of composite collagen prostheses designed for ligament reconstruction. J. Orthop. Res. 12(1):128-137.
- Maxian SH, Zawadsky JP, Dunn MG (1994) Effect of Ca/P coating resorption and surgical fit on the bone/implant interface. J. Biomed. Mater. Res. 28(11):1311-1319.
- Dunn MG, Avasarala PN, Zawadsky JP (1993) Optimization of extruded collagen fibers for ACL reconstruction. J. Biomed. Mater. Res. 27(12):1545-1552.
- Maxian SH, Zawadsky JP, Dunn MG (1993) Mechanical and histological evaluation of amorphous calcium phosphate and poorly crystallized hydroxyapatite coatings on titanium implants. J. Biomed. Mater. Res. 27(6):717-728.
- Maxian SH, Zawadsky JP, Dunn MG (1993) In vitro evaluation of amorphous calcium phosphate and poorly crystallized hydroxyapatite coatings on titanium implants. J. Biomed. Mater. Res. 27(1):111-117.
- Dunn MG, Tria AJ, Kato YP, Bechler JR, Ochner RS, Zawadsky JP, Silver FH (1992) Anterior cruciate ligament reconstruction using a composite collagenous prosthesis. A biomechanical and histologic study in rabbits. Am. J. Sports. Med. 20(5):507-515.
- Dunn MG, Maxian SH (1991) Hydroxyapatite-coated orthopedic implants. J. Long. Term. Eff. Med. Implants. 1(2):193-203.
Contact Us
Department of Orthopaedic Surgery
Medical Education Building, Room 425
Robert Wood Johnson Medical School
51 French Street
New Brunswick, NJ 08901
Phone: 732-235-7869
Fax: 732-235-6002
