Pediatric Residency
Overview of the Program
The pediatric residency program at Robert Wood Johnson Medical School prepares residents for any specialty in pediatrics whether in private practice, academic medicine, or a sub-specialty, accomplished through a comprehensive educational experience and broad exposure to clinical pediatrics. The Department of Pediatrics is housed within the Child Health Institute of New Jersey, the cornerstone of the children's academic health campus adjacent to the institute’s research facilities, the Bristol-Myers Squibb Children's Hospital at Robert Wood Johnson University Hospital, and PSE&G Children's Specialized Hospital, both of which are part of RWJ Barnabas Health. Together, they form a unique partnership of world-class institutions representing an exciting opportunity for collaboration and improved pediatric care.
Program Highlights
- Residents are involved in the direct care of pediatric patients, both outpatient and inpatient; on the children’s hospital’s general floor and intensive care unit; and from primary to tertiary care
- Protected learning time for academic half-day, morning reports, case conferences and grand rounds
- UpToDate and Lexicomp access
- Medical school library with extensive electronic resources
- Our program transitioned to the X+Y curriculum in July 2022
- Clinical training complemented by a curriculum designed to develop the skills a pediatrician requires, as a patient advocate, educator and researcher
- Membership in the American Academy of Pediatrics with access to pedialink learning center
- New England Journal of Medicine pediatric board preparation program
- Emphasis on individualized curriculum
Reasons for Choosing Robert Wood Johnson Pediatric Residency Program
- An integrated program utilizing a university hospital and an academically oriented community hospital.
- Busy clinical services with a large variety of patients.
- All pediatric subspecialties represented on the full-time faculty.
- Graduated responsibility and independence.
- Wide diversity of outpatient experience, including primary and subspecialty care.
- Excellent ancillary staff
- Faculty dedicated to giving their patients state of the art and compassionate medical care, and to instill these qualities in students and residents.
- Supportive environment with open relationships between residents and faculty.
- Regional Children's Center offering care across the entire clinical spectrum
- Stimulating case conferences.
- Nationally renowned Institute for the Study of Child Development and Boggs Center.
- Research opportunities and support.
- Professional, dedicated nursing and ancillary staff who work collaboratively with pediatricians.
Residency and fellowship programs training at Robert Wood Johnson Medical School benefit from the resources and interprofessional opportunities available through the Rutgers Health institutional sponsorship. Learn more about all of the Rutgers Health sponsored graduate medical education programs on our sponsoring institution webpage.

Welcome to our pediatric residency program! Our residents are the heart of our department. Their vitality, curiosity and dedication to our patients reminds the faculty daily why we chose this profession. Our residents are a diverse and ambitious group headed by our dedicated medical education leaders. As you embark on this journey of apprenticeship, know that we will be there to help you succeed. Your success equates directly to ours!
In fact, one of our goals is to create a program where you will want to come back and work alongside us. Our program is unique in that we are centralized in a strong Children’s Health campus where you can explore your various interests. The partnerships between the Department of Pediatrics of RWJMS and Child Health Institute of New Jersey, Bristol-Myers Squibb Children's Hospital at Robert Wood Johnson University Hospital, and PSE&G Children's Specialized Hospital along with the many partners of Robert Wood Johnson Barnabas Health opens the door to exploration of many career paths.
Whether you wish to go into primary pediatric care or a subspecialty, whether your track is advocacy, global, or research, know that we will help you become proficient in that area (or) in your dream area. We are growing our clinical and research programs, and I invite you to join us during this exciting journey ahead! Along the way, both residents and faculty will enrich each other through shared experiences and skills – promising a fun journey for you!
Vikas Dharnidharka, MD, MPH
Chair and Professor of Pediatrics
Who We Are
-
Vikas Dharnidharka, MD, MPH
Chair and Professor of PediatricsJoann Carlson, MD
Associate Professor of Pediatrics
Residency Program Director
joann.carlson@rwjms.rutgers.eduThank you so much for visiting our website! We are so excited to share with you the highlights of our residency program. As the world around us is changing, we are ready to face the new challenges of residency training and building virtual learning curriculums. Our main goal continues to be to train excellent, well-rounded, and dedicated pediatricians.
My favorite part of our program is certainly the people. We have amazing faculty in all of the subspecialties who are not only astute clinicians but also incredible educators who love to teach. We also are so lucky to have extraordinary residents. Our residents continue to impress me throughout their training with their dedication to their patients, to learning and to each other. It is privilege to both teach and mentor them. We see their hard work paying off when they become true leaders in both general pediatrics and the subspecialities. Our graduates are one of the best ways to measure our program’s success. Please review our website but I encourage you all to contact us for more information and any questions you have. I am thrilled to be the program director and hope through this website you can start to see why I love being a leader in the residency program at RWJ/Rutgers. Thank you for your time and I look forward to hearing from you!
Natalie Torres-Feliz, MD
Assistant Professor of Pediatrics
Associate Program DirectorWelcome to our website! We are so excited to share with you all the exciting opportunities that we have in our program. We have a diverse resident physician population that reflects the population that we care for in the New Brunswick area. Our close knit team of attending physicians are able to form close working relationships with resident physicians. One of the strong points of our program is the group of physicians and nurses that make this program a close-knit and welcoming learning environment. I look forward to discussing with you all more about how we provide inclusive patient care and graduate strong, well-rounded pediatricians.
Joanne Edwards Algranti
Residency Program Coordinator
jde59@rwjms.rutgers.eduMona Matta
Residency Program Coordinator
mona.matta@rwjms.rutgers.edu -
Chief Residents


PGY1 Residents:
Zachary Anderson, MD
St. George's University School of Medicine
Henry Chen, MD
Rutgers New Jersey Medical School
Emily Costello, MD
Rutgers RWJMS
Vanessa Freedman, DO
Des Moines University College of Osteopathic Medicine
Shery Galkin, MD
St. George's University School of Medicine
Sarah Nagy, MD
Rutgers RWJMS
Meera Navadia, DO
Nova Southeastern University Dr. Kiran C. Patel College of Osteopathic Medicine
Dhruva Nilakantan, MD
Royal College of Surgeons in Ireland School of Medicine
Allison Pilon, MD
St. George's University School of Medicine
Stefanie Zarelli, MD
Rutgers New Jersey Medical School
Raisa Zahir, MD
Wayne State University School of Medicine

PGY-2 Residents
- Kristina Beluskov, DO - Nova Southeastern University Dr. Kiran Patel School of Osteopathic Medicine
- Leigh Ann Nicole Boyle, MD - Rutgers NJMS
- Saakshi Ramesh Daswani, MD - Royal College of Surgeons in Ireland
- Erica Levin, MD Rutgers - RWJMS
- Iswarya Manivannan, MD - Sidney Kimmel College at Thomas Jefferson University
- Bao-Nghi Nguyen, MD - Royal College of Surgeons in Ireland
- Lawrence Paffini, MD - New York Long Island School of Medicine
- Jessenia Palacio-Meadows, MD - Rutgers NJMS
- Alyssa Shannon, DO - Touro College of Osteopathic Medicine-Middletown
- Abir Thakur, MD - Renaissance School of Medicine at Stony Brook University
- Kristin Upton, DO - Lake Erie College of Osteopathic Medicine

PGY-3 Residents
- Darlene Ashamole, MD - Howard University School of Medicine
- Simren Chotai, MD - Royal College of Surgeons in Ireland
- Michaela Creus, MD - New York Medical College
- Lalita Ganti, MD - Cooper Medical School of Rowan University
- Shayna Glassberg, DO - Touro College of Osteopathic Medicine
- Mona Khan, DO - Rowan University College of Osteopathic Medicine
- Konstandina Kokinakos, DO - Touro College of Osteopathic Medicine
- Anmol Kundlas, MD - USF Health Morsani College of Medicine
- Charles Li, MD - SUNY-Upstate School of Medicine
- Anthony Poltronetti, MD - Lewis Katz School of Medicine at Temple University
- Aline Sandouk, MD, PhD - University of Iowa College of Medicine
Resident Support Services
Members of the faculty take an active and ongoing interest in resident well-being.
Mentorship and support services include:
- Individual faculty advisor and scholarly activity mentor
- Regular meetings with the director of the residency program
- Monthly town hall meeting
- Resident retreats, held twice a year, and organized by class
- Open-door policy of the chair and faculty
- Annual year-end residents' day off
- Year-end dinner for residents, fellows and aculty
- Back-up residents for sick call
- Parental leave policy
- Resident Wellness Program
- Resident Assistance Program
- Career development support
- Complementary access to Cognitive Skills Center
-
Where They Went
Graduates 2025
- Sarah Andrea, MD - PICU Fellow at Westchester Medical Center Children’s Hospital
- Katherine Briski, MD - Pediatric Emergency Medicine Fellow at Nemours Children’s Hospital
- Sameera Chaudhry, MD - Pediatric Emergency Medicine Fellow at Rutgers NJMS
- Jordana Gross, MD - General Pediatrics, New York
- Adam Halpern, DO - Chief Resident then General Pediatrics, New Jersey
- Axel Ivander, MD - Pediatric Emergency Medicine Fellow at Johns Hopkins Children’s Center
- Bahaa Labib, MD - Pediatric Endocrinology Fellow at Children’s Hospital of Philadelphia
- Casey Lamar, MD - PICU Fellow at Yale Children’s Hospital
- Bethany Murphy, MD - Chief Resident
- Keisha Target, MD - Pediatric Emergency Medicine Fellow at Johns Hopkins Children’s Center
- George Ye, MD - Pediatric Hematology Oncology Fellow at Memorial Sloan Kettering Cancer Center

Graduates 2024
- Soheil Afsharpour, MD - Chief Resident then Cardiology Fellow at University of British Columbia
- Diane Algava, MD - Emergency Medicine Fellow and Urgent Care at Phoenix Children’s Hospital
- Ezra Chefitz, MD - Gastroenterology Fellow at University of Pittsburgh Medical Center
- Patricia Hoffman, DO - Rheumatology Fellow at Weill Cornell Medical Center/Hospital for Special Surgery
- Samanta Mukkamala, MD - Emergency Medicine Fellow at Wake Forest Baptist Health
- Gabriel Munoz, MD - General Pediatrics, New York
- Christina Nashed, DO - General Pediatrics, New Jersey
- Jessica Ohiri, MD - Anesthesiology Residency at Rutgers NJMS
- Christopher Ramirez, MD - General Pediatrics, New York
- Sruchika Sabu, MD - Endocrinology Fellow at University of Michigan
- Pardeep Sidhu, MD - Consultant Pediatrician and Fast Track Attending, Toronto, Canada

Graduates 2023
- Abigail Bergman, MD - Chief Resident then Pulmonary Fellow, CHOP
- Bianca Chendrimada, DO - PM Pediatrics
- Yisha Cheng, MD - Emergency Medicine Fellowship, St Christopher’s Hospital for Children
- Matthew Federici, MD - Cardiology Fellowship, Nicklaus Children’s Hospital
- Lori Fingerhut, MD - Endocrinology Fellowship, Children’s National Medical Center
- Jazmin Garcia, DO - Chief Resident then PICU Fellowship, Baylor
- Sally Ng, MD - General Pediatrics
- Haidang Nguyen, MD - General Pediatrics
- Sonia Pothraj, MD - General Pediatrics
- Sara Rouff, DO - General Pediatrics
- Soraya Simon, MD - General Pediatrics

Graduates 2022
- Seherisch Ahmad, MD - Chief Resident, Emergency Medicine Fellowship, Rutgers NJMS
- Kathrine Baldwin, DO - Pulmonary Fellowship, Westchester Medical Center
- Avram Bursky-Tammam, MD - PICU Hospitalist, Cohen's Children's Medical Center
- Perel Bursky-Tammam, MD - General Pediatrics
- Gabrielle Capozzoli, MD - General Pediatrics
- Chika Esochaghi, MD - Chief Resident, Nursery Hospitalist in Maryland
- Michelle Gaglia, DO - Anesthesia Residency, Rutgers Robert Wood Johnson Medical School
- Courtney Greene, DO - Sports Medicine Fellowship, Rainbow Babies & Children's Hospital
- Daniel Helfgott, MD - Neonatal-Perinatal Fellowship, Stony Brook Children's Hospital
- Lauren Sall, DO - General Pediatrics, California
- Alexandria Speakman, DO - Gastroenterology Fellowship, Cincinnati Children's Hospital

Graduates 2021
- Marianne Armanious, MD - General Pediatrics, New Jersey
- Madhusree Chowdhury, MD - General Pediatrics, Connecticut
- Samantha Chu, DO – Fellowship in Hematology/Oncology at Memorial Sloane Kettering
- Rannan Kased, DO – Fellowship in Neonatology at Sparrow Hospital, Michigan State University
- Jovanna Madray, DO - General Pediatrics, New Jersey
- Emily Negroponte, MD - General Pediatrics, New Jersey
- Akreeti Maskey-Pagodin, MD-Chief resident then General Pediatrics, New Jersey
- Lauretta Oseni, MD- Hospitalist, NYU then Fellowship in Hospitalist Medicine at SUNY Downstate
- Aashiki Shah, DO - General Pediatrics, New Jersey
- Peter Wu, MD - Urgent Care Fellowship at Children’s National Medical Center
- Sarah Yavelberg, MD - Chief resident then Hospitalist/General Pediatrics, New Jersey

Graduates 2020
- Tolu Ariyo, MD – General Pediatrics, Maryland
- Amy Cheng, MD – General Pediatrics, Maryland
- Jaya Isaac, MD - Chief Resident then Fellowship in Pediatric Nephrology at Children’s Hospital of Montefiore
- Maaz Jalil, DO – Fellowship in Allergy and Immunology at Case Western Reserve University
- Peter Jang, MD - Radiology Residency, Cooper Medical School of Rowan University
- Carolyn Ochoa, MD - Newborn Nursery Hospitalist, NYP Weill Cornell Medical Center
- Mehrin Sadiq, MD – General Pediatrics, Virginia
- Shivani Shah, DO – Fellowship in Pediatric Emergency Medicine at Newark Beth Israel
- Karen Teoh, MD – General Pediatrics, Brooklyn NY
- Debra Zharnest, MD - Chief Resident then Fellowship in Pediatric Emergency Medicine at St Christopher’s Hospital for Children
Benefits and Salary
Our residency and fellowship programs offer a uniform package of benefits consistent with those provided at all graduate medical educational programs operated by the medical school. Full details regarding benefits and salary are continuously updated by the Office of Graduate Medical Education.

Curriculum
-
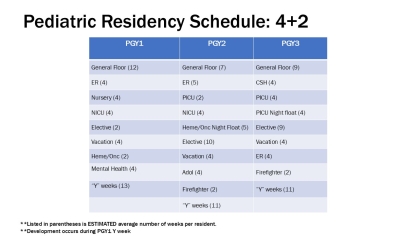
The focus of the first year (PGY-1) is to differentiate between well, ill- appearing, and critically ill children. Four months of the year are spent in the inpatient setting at BMSCH. Additional time is spent learning about newborns both in the well-baby unit and in the neonatal intensive care unit.
The second year (PGY-2) lets the resident begin to take on leadership roles in the inpatient setting. Further, the resident is able to start exploring various areas of pediatrics that he/she believe will be helpful in his/her future with several months tailored to individual needs. The resident spends block time in the intensive care units and in the emergency department.
The final year (PGY-3) encourages residents to take ownership of their year developing an individualized curriculum that meets both their educational needs as well as their career goals. Opportunities for electives and completing their individualized curricula are the primary emphasis. However, residents also spend time as the inpatient senior for two blocks, and an additional two blocks in the intensive care unit.
In July 2022, our program transitioned to the X+Y scheduling system. We are using a 3 +1 model and have officially joined the ACGME pilot for pediatric programs. With this system, residents spend 3 weeks in an “X” rotation and then have one “Y” week of outpatient experiences that can include continuity clinic, advocacy, development, research and administrative time. Overall, this scheduling system has been shown to lead to improvements in patient care, educational outcomes and the clinic experience.
For their clinic experience, residents are assigned to either Eric B Chandler Health Center or Robert Wood Johnson Medical Group at Somerset. Accompanying the continuity clinic experience is a well-organized curriculum that rotates and repeats over the course of the residents’ training. During years one and two all residents are required to see general pediatric patients at their primary care continuity site. However, if residents are pursuing subspecialty training and they wish to have a continuity experience in their subspecialty, they are able to arrange an outpatient longitudinal clinic in that venue.
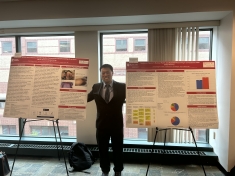
All residents participate in a quality improvement (QI) curriculum and participate in QI workshops during block lecture. In addition, all residents are required to complete a scholarly project.
-
-
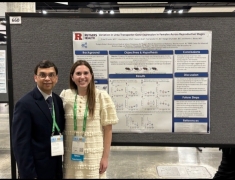
In addition to teaching and clinical activities, faculty, fellows and residents are involved in clinical and bench research. Residents are required to complete a scholarly activity prior to graduation. Projects involving quality improvement and community advocacy have been completed to fulfill this requirement and opportunities in the Pediatric Clinical Research Center, located within the Child Health Institute, are available to residents.
-
- Newborn Vitamin K Refusal Rates and Parental Reasoning.
- Improving Inpatient Management of Eating Disorders
- Childhood Obesity: A QI Project
- ASD and PTSD in English and Spanish Speaking Parents of Children admitted to the Pediatric ICU and General Pediatric Wards
- Association Between Paternal Depression in the First Year of Life and Father Absence from the Home During Childhood
- Parental Food Allergy Survey
- Prospective Study of GVHD in Pediatric BMT
- Survey of VTE Protocols for Risk Assessment
- CHPG Hypoxemia Murine Model
- Utility of Video Telehealth Implementation in Transport
- Project LIGHT
- Reducing Pressure Injuries in the PICU
- Improving Inpatient Management of Eating Disorders
- Parental Food Allergy Survey
- Prospective Study of GVHD in Pediatric BMT
- Survey of VTE Protocols for Risk Assessment
- Erythromycin Microbiome Project
- QOL Assessment for Peds Endo Patients
- CHPG Hypoxemia Murine Model
- Asynchronous Literacy Boost
PGY3:
- Transport Study- Telehealth QI Project
- Necrotizing enterocolitis (NEC) in extremely preterm neonates: Risk factors and Outcomes
- Transitional Care for Diabetic Adolescents
- A pilot study of propranolol to treat behaviors in adolescents
- Outcomes and effectiveness of enteral nutrition in IBD patients
- Validating Claims of Juvenile Idiopathic Arthritis
- Reach Out & Read: Implementation Among Pediatric Residents
- The Characterization of PICC Line Displacement by Upper Extremity Manipulation via Point of Care Ultrasonography
- Prognostic use of anti-TPO and anti-thyroglobulin antibodies in children with Autoimmune Thyroiditis
PGY2:
- Utility of Video Telehealth Implementation in Transport
- Project LIGHT
- Reducing Pressure Injuries in the PICU
- Improving Inpatient Management of Eating Disorders
- Parental Food Allergy Survey
- Inpatient Management of Eating Disorders
- Prospective Study of GVHD in Pediatric BMT
- Survey of VTE Protocols for Risk Assessment
- Erythromycin Microbiome Project
- QOL Assessment for Peds Endo Patients
- CHPG Hypoxemia Murine Model
- Asynchronous Literacy Boost
Contact Us
Pediatric Residency
Child Health Institute
89 French Street
New Brunswick, NJ 08901
Phone: 732-235-7883
Fax: 732-235-6609
Twitter: @PedsRWJ
Instagram: @RutgersRWJPedsResidents
Joann Carlson, MD
Associate Professor of Pediatrics
Program Director
joann.carlson@rwjms.rutgers.edu
Natalie Torres-Feliz, MD
Assistant Professor of Pediatrics
Associate Program Director
torresns@rwjms.rutgers.edu