
A Publication for Alumni & Friends of Rutgers Robert Wood Johnson Medical School

From Adoption Medicine to Solving Diagnostic Dilemmas, Expanded Pediatric Services Keeps Kids Close to Home for Care
“You’d be surprised how few medical programs for children exist in this part of New Jersey. It’s unconscionable,” says Sally Radovick, MD, chair and professor, Department of Pediatrics, and senior associate dean for clinical and translational research at Robert Wood Johnson Medical School.
Despite being one of the country’s most populated areas, central New Jersey has a dearth of specialized medical services for children. To bridge the gap and ensure that patients and their families don’t have to travel for treatment, the Department of Pediatrics has developed several destination services to support young patients and their families. Through innovative services like its international adoption clinic and diagnostic referral service, patients have access to state-of-the-art care right at home.

Taking Some of the Guesswork Out of International Adoption
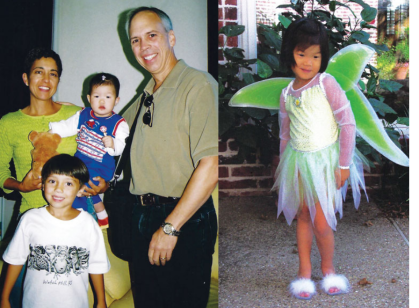
When pediatrician Susan Dibs, MD, adopted her daughter from China in 2004, she knew that her personal life would change dramatically. She didn’t know the impact the experience would have on her professional life, too.
Typically, when someone wants to adopt a child internationally, he or she works with a licensed adoption agency that tries to match them with an appropriate child based on the adopters’ preferences. Most children available for adoption have special needs, whether medical, psychological, or developmental, which can range from mild to severe. Once adoptive parents are matched with a child, the agency will provide a referral—a medical report about the child’s birth, medical history, growth patterns, and physical examination. In many cases, adopters are required to have these records reviewed and interpreted by a physician in the United States before making a decision about the placement. However, not all physicians are versed in this type of consultation and the nuances of foreign medical care.
To fully understand the medical review process during her adoption experience, Dr. Dibs researched common health conditions facing children in underdeveloped countries, including infectious diseases, malnutrition, and developmental and behavioral issues, and how American doctors can screen for these conditions using foreign medical data. Dr. Dibs found this research so interesting that she refocused her career on the medical issues associated with international adoption.
“It means a lot to adopting families that I’ve been through the process,” explains Dr. Dibs, an associate professor of pediatrics, and director of international adoption medicine at Robert Wood Johnson Medical School and attending physician at Bristol-Myers Squibb Children’s Hospital at Robert Wood Johnson University Hospital. “It can be reassuring to them since I have experienced a lot of what they are going through first hand.”
Before joining the medical school faculty in August 2021, Dr. Dibs developed international adoption medical clinics in Texas and Maryland. Now, Rutgers Health, under the leadership of Dr. Dibs, is home to the only medical review program of its kind in the state.
Through the new clinic, Dr. Dibs reviews records and reports her findings to families by phone or videoconference. Once children come to live in the United States, the clinic can perform comprehensive post-arrival exams and diagnostic testing to check for conditions common to this population. Children identified to have a condition that requires subspecialty care are referred to the appropriate subspecialist.
Patients are referred to the clinic here from international adoption agencies, independent social workers, and local and national community support groups. However, most referrals come through word of mouth.
“It’s important to find a doctor who is knowledgeable about medical records from other countries and the common conditions found in those countries,” Dr. Dibs explains. “It’s not knowledge that most pediatricians have.”
Dr. R., a pediatrician in New York City who is in the process of adopting a child from India, agrees.
“You have to look through a pile of paperwork and try to decide if this child should be yours,” she says. “It’s surreal, emotional, and complicated. You have to make a decision based on limited information, including diagnostic tests that don’t match the standards you see here in the U.S.”

Dr. R. was referred to the International Adoption Clinic for help deciphering medical data on potential adoptive matches. Despite her background, she found that understanding an infant’s medical status required not just interpreting test results but also knowing what information was missing from a report that could be requested to paint a clearer clinical picture.
“Dr. Dibs provides a set of impartial eyes for me,” Dr. R. explains. “She can see what is—and isn’t—represented by the data.”
And once Dr. R. brings her child home, Dr. Dibs will perform a comprehensive examination to
assess the child’s health status further. If the infant requires advanced medical care, Dr. Dibs will provide referrals to clinical specialists.
“I like that Dr. Dibs is affiliated with an academic institution,” Dr. R. says. “There’s a level of connectedness in academia that will be helpful if my child needs a higher level of care.”
Pediatrics Department Expands Specialized Services
For patients with difficult-to-diagnose conditions, the Diagnostic Referral Service provides access to an array of expert pediatric subspecialists. The clinic is overseen by pediatrician Joann Alfonzo, MD, assistant professor, Department of Pediatrics, and caters to children who have illnesses that are “diagnostic dilemmas.”
“There are childhood illnesses, such as multisystemic disorders, where it’s not clear if the issue is cardiac, GI, or something else entirely,” Dr. Radovick explains. “Our diagnostic clinic provides expert care to patients who have illnesses that are difficult to diagnose or require multispecialty care. It has become a destination program because there’s nothing else like it anywhere else in the state.”

One such confounding condition is multisystem inflammatory syndrome in children (MIS-C), which can cause inflammation of the heart, lungs, kidneys, brain, skin, eyes, or gastrointestinal organs. While much is still unknown about the condition, it appears to be linked to COVID-19. Lawrence C. Kleinman, MD, MPH, professor and vice chair for academic development and chief, Division of Population Health, Quality, and Implementation Science in the Department of Pediatrics, was recently awarded a two-year, $1.6 million grant from the National Institutes of Health to study the syndrome. The project will focus on identifying the factors that may help predict which children are at greatest risk for serious illness from SARS-CoV-2 infection, the virus that causes COVID-19.
In addition, the medical school’s Pediatric Clinical Research Center, which helped pioneer clinical trials on the efficacy of a COVID-19 vaccine for children ages 5 to 17, is investigating a preventive vaccine for children under 5.
“There was a time when people thought that COVID was not a pediatric disease, but the omicron variant has taught us differently. Unfortunately, the virus continues to ravage children,” Dr. Radovick says. “It has put a great clinical strain on our services. However, because we were involved at the very early stages of the disease, we have a breadth of knowledge about treating COVID-19 that we can share locally, nationally, and internationally.”
The Pediatrics department also has expanded a number of other clinical services. Barrie Cohen, MD, assistant professor of pediatrics, is providing new allergy and immunology services for children. Sari Bentsianov, MD, assistant professor of pediatrics, is expanding the services offered by the Adolescent Medicine Program. Ian Marshall, MD, associate professor of pediatrics and director of the Division of Endocrinology, directs a comprehensive transgender program that provides ongoing compassionate care to 400 transgender teens.
Lastly, with the addition of new leaders in critical care medicine, associate professor Simon Li, MD, and professor Vadim Ten, MD, in neonatology, the department has been able to expand its inpatient pediatric extracorporeal membrane oxygenation services to ensure critically ill children don’t need to be transported to another facility for lifesaving care. Instead, these patients can be referred to Bristol-Myers Squibb Children’s Hospital, which operates the region’s only pediatric intensive care unit staffed 24/7 by in-house pediatric critical care physicians.
From specialty services such as the international adoption and diagnostic clinics to comprehensive pediatric inpatient, primary, and subspecialty care, children and families in New Jersey and beyond are in good hands with the experts at Robert Wood Johnson Medical School.
