
A Publication for Alumni & Friends of Rutgers Robert Wood Johnson Medical School
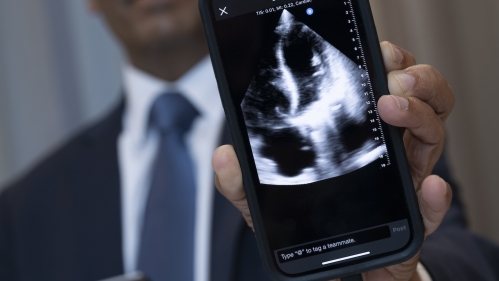
Innovations in Cardiac Imaging: Ultrasound as the Ultimate Diagnostic Tool

When cardiologist Partho Sengupta, MD, FACC, joined Rutgers Robert Wood Johnson Medical School and Robert Wood Johnson University Hospital (RWJUH) in July 2021, he brought with him an insatiable drive for innovation and inquiry. As the Henry Rutgers Professor of Cardiology and chief of cardiology, his goal is to create a hub of innovation here that leverages new technologies—including artificial intelligence (AI) and advanced imaging—to improve diagnosis, better tailor treatment, and, ultimately, improve patient outcomes.
“Empathy and connection are dying out in the modern world. With AI and machine learning, we can focus on the personalized, human side of medicine,” Dr. Sengupta says. “The more specific information we can provide to our patients and the more data-driven decisions we can make regarding their care, the more comforted and convinced patients will be about our ability to manage their care.”
Previously at the West Virginia School of Medicine and WVU Heart and Vascular Institute, Dr. Sengupta is working closely with Anthony Altobelli, MD, clinical chief of cardiology, RWJUH, and Mark Russo, MD, associate professor of surgery and chief of the Division of Cardiac Surgery at the medical school, and chief of cardiovascular and thoracic surgery, RWJUH, to lead one of the largest cardiovascular and thoracic services in the region. He is a vocal advocate for using ultrasound imaging at the bedside both in the United States and in low-income countries to detect cardiovascular disease at its earliest, most treatable stages.
The Sounds of Silent Disease
“Imaging is the window to understanding the heart. Sound and its reflection are extremely powerful sources of diagnostic information,” Dr. Sengupta explains. “We’re at the beginning of a new understanding about the heart’s muscles and how they function over time. Without imaging, you can’t imagine. Imaging enables more powerful exploration of the heart and allows us to take innovation one step further.”
With AI and machine learning, we can focus on the personalized, human side of medicine. The more specific information we can provide to our patients and the more data-driven decisions we can make regarding their care, the more comforted and convinced patients will be about our ability to manage their care.
Partho Sengupta, MD, FACC
Currently, cardiologists evaluate patients using stethoscopes, medical history, electrocardiogram (ECG), and old-fashioned conversation. These methods don’t allow physicians to assess the structure and function of the heart’s chambers and valves to detect or rule out major disease, according to Dr. Sengupta. For example, physicians may hear abnormal heart sounds in a patient but then must determine the specific defect only using a stethoscope. And while ECG can detect heart disease, it’s not as sensitive as ultrasound. These factors contribute to unnecessary referrals for downstream testing.
However, with ultrasound, sound is reflected to develop moving pictures of the heart’s chambers, walls, valves, and blood flow. Using the technology, clinicians can detect chamber enlargement, reduced squeeze in motion (dysfunction), congenital heart disease, and valve blockages and leaks.
In the future, says Dr. Sengupta, cardiologists carrying pocket-sized, handheld ultrasound units will scan asymptomatic yet high-risk patients during routine office visits. From an external scan, cardiologists can see the heart’s structure and function in detail in just a matter of minutes. Then, AI algorithms and machine learning will translate the highly complex, “hidden” ultrasound data to uncover silent disease. Combined with traditional electrocardiogram testing and other tools, this data will predict the progression of cardiovascular disease, such as the patient’s risk of future heart failure, and inform proactive care to minimize that risk.
“Patients are looking for information when they see the doctor,” Dr. Sengupta explains. “With ultrasound, you have instant answers.”

To test his theory, Dr. Sengupta is piloting a program funded by a Bridges in Digital Health grant from the National Science Foundation. The program promotes using pocket ultrasound in place of a stethoscope during patient rounds. He is training cardiac fellows how to use pocket ultrasound and is working with Rutgers University’s Engineering Department to develop the AI parameters needed to translate ultrasound data in data points, such as ejection fraction. AI also helps ensure images are accurately acquired even by those without a lot of experience by guiding the movement of the scanning transducer. This improves image quality and reduces variability.

To increase patient access to ultrasound imaging, he also is exploring the use of robotics to capture images at places like pharmacies and rural clinics. A robotic arm would acquire images, and then that information would be securely transmitted to a cardiologist for reading. Engineers from France are helping install at the medical school the first U.S. Food and Drug Administration–approved robotic ultrasound system for clinical use in the United States, according to Dr. Sengupta.
A Look Further into the Future of Cardiovascular Care
Beyond the precision medicine that ultrasound imaging, AI, and machine learning enable, Dr. Sengupta and his team are researching the physiological signals captured by wearable digital technologies, such as Fitbits, Apple watches, and remote ECG monitors, and how this data can further guide clinical decision making.
“We want to understand each individual’s phenotype and the diversity of how cardiovascular diseases present so we no longer give homogenized treatment,” Dr. Sengupta explains. “We want to identify the best therapeutic option based on that person’s specific characteristics.”
The ultimate goal is to create an academic center to train the next generation of leaders in cardiovascular medicine and help the 18.2 million American adults who suffer from cardiac disease, the leading cause of death in the United States.
“The medical school and hospital are working together to create an ecosystem for innovation,” he says. “We’re removing the barriers to creative thinking, encouraging fearless questioning, and investing in the future to develop an environment of inquiry. Together, we will question the status quo and find ways to move cardiovascular medicine forward.”
